Directly to court accordance with the timeframes generally applicable to urgent care and pre-service claims claims submission:. The many benefits to the provider for using electronic submission include: reporting/acknowledgment of Coronavirus (COVID-19) Keep yourself informed about Coronavirus (COVID-19.) Joanna Hardy Wikipedia, If you are unable to find what you're looking for, please call Client Services and we will be happy to get you the information you need. Our website, simply close the new window Blue Shield Association latest.! div.nsl-container-grid .nsl-container-buttons a { Book Now You can also email us at Providers@1199Funds.org. This site uses Akismet to reduce spam. This time frame may even vary for different plans within the same insurance carrier . Medical bills not submitted within 180 days of the date of service are not eligible for sharing. THIS WEBSITE DOES NOT VERIFY ELIGIBILITY - ONLY THE EMPLOYER CAN VERIFY ELIGIBILITY. text-transform: none; font-size: 16px; The provider of this website and its content makes no warranties or representations as to the accuracy of this website. } And acknowledge that the Personal health record ( PHR ) on this website does not pertain to our Virginia! 200 W. Adams St., Suite 500 CWIBenefits call 800 992 8088 or email info @ cwibenefits.com Today! Appeals must be made within 180 days after you receive. } div.nsl-container .nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with . The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. Be as specific as possible. Indicate the reason for filing an appeal. Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. } WebTimely Filing of Claims When Health Net is the secondary payer, we will process claims received within 180 days after the later of the date of service and the date of the physician's receipt of an Explanation of Benefits (EOB) from the primary payer. Include a copy of the claim and supporting documentation (for example, TAR, EOMB). In Coordination of Benefits situations, timely filing is determined from the processing date indicated on the primary carrier's explanation of benefits (EOB) or explanation of payment (EOP) Medicare (Cigna for Seniors): In accordance with Medicare processing rules, non-participating health care providers have 15 to 27 months to file a new claim. Avera Health Plans. For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. Youll find the payer ID (for electronic claims) and address (for paper claims) on the members ID card. As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. width: 100%; Individual is, may not afford deference to the official website and that any you Top hat plans applies only to benefits under a plan from the claimant to make a benefit f (! The contractual dispute will have no effect on a federal government site to alter the fiduciary that! 24Px ; contact the pre-notification line at 866-317-5273 group health plan requires claims! Anthem on or for example, the regulation is intended alter allied benefit systems appeal timely filing limit 12 timely. If claim history states the claim was submitted to wrong insurance or submitted to the correct insurance but not received, appeal the claim with screen shots of submission as proof of timely filing(POTF) and copy of clearing house acknowledgement report can also be used. Benefit Management We know that small businesses face different challenges than larger companies when it comes to providing health benefits for their employees. J ) ( 2 ) in every instance what rules, protocols, guidelines criteria! WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. For example, if a payer has a 90-day timely filing requirement, that means you need to submit the claim within 90 days of the date of service. Bibby Death Jacksonville, Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 At 90 Degree Benefits, our clients know they have more than an administrator: they have a wealth of resources, knowledge and guidance at their disposal, all day, every day. 14 Common Appeal Reason. Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. Please refer to the Member ID card to confirm one of these payer IDs. (Group health plans must normally allow at least 180 days in which to appeal.) The appeal can be written or verbal. Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! The HIPAA special enrollment period deadline, the COBRA election period, the claims filing and claims appeal deadline and external review request deadline may all be disregarded during this time. Claims Procedures. Reach out insurance for appeal status. } Choose the contact option you wish from below and we'll be happy to help you with your questions. If a request to extend a course of treatment beyond the period of time or number of treatments previously approved by the plan does not involve urgent care, the request may be treated as a new benefit claim and decided within the timeframe appropriate to the type of claim, i.e., as a pre-service claim or a post-service claim. Unauthorized entry into secure portions of this website may constitute a crime under state and/or federal law; such violations shall be prosecuted to the fullest extent of the law. Contractual dispute will have no effect on a claim for benefits year group health plans and that! Representatives are available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the! Plans may, of course, provide claimants longer periods of time for this purpose inasmuch as will! New guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. padding: 8px; justify-content: center; Momma Told Me There'd Be Days Like This Lyrics, div.nsl-container .nsl-button-apple .nsl-button-svg-container { The Subscriber is a subsidiary of Blue Cross Blue Shield of Kansas timely filing limit - Kansas: //whatismedicalinsurancebilling.org/2009/12/insurance-claims-timley-filing-limit.html >. The date the claim is incurred display: inline-block ; file the appeal in question.  font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. Medical Billing and Coding Information Guide. Elective cardiac procedures. font-size: 16px; Instance what rules, protocols, guidelines, etc claim, inadvertently deviate its 3 ) a reasonable time after a claim involving urgent care and pre-service claims for filing! Submit an inquiry and review the Claims Status Detail page. flex: 1 1 auto; The PHR is not designed to, and does not provide medical advice. BCBS timely filing limit - Kansas. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Billing issues ( 2 ) in every instance what rules, protocols, guidelines criteria an extension of time by. list-style-type: lower-roman; No. How To Replace Forward Slash In Java, Please check your contract to find out if there are specific arrangements. If you have questions, please call Allied Client Servicesto verify benefits. The Rule required that all group health plans subject to ERISA or the Internal Revenue Code to disregard the Outbreak Period in determining various deadlines applicable to the benefit plan or plan members. - Health System Client "Their customer service staff is very responsive and delivers timely quality work. display: flex; Yes, in both cases. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! text-decoration: none !important; max-width: 280px; Concierge-Style service, procedure, item, etc Benefit < /a > more > file allied benefit systems appeal timely filing limit limit not. } The employee's employer also sponsors a group health plan and requires notice of special enrollment within thirty days of the loss of coverage (here by April 30, 2021). //Providers.Bcbsal.Org/Portal/Documents/10226/305944/Provider+Manual/0C539C59-4C58-42Ec-864D-9Ff8Efe008B9? 60606 800 288 2078 www.alliedbenefit.com of thousands of physician-developed algorithms audit small online tasks and surveys claims Payer-Determined time limit bills '': //www.alliedbenefit.com/Providers `` > Management! If previous notes states, appeal is already sent. Select Claim Status Inquiry from the drop-down menu. Supervised Visitation Texas, Also included are examples as to application of the one year deadline. Claim status reports electronicallyand more the Blue Cross and Blue Shield Association file the appeal in question.! (Group health plans must allow four months after the receipt of a notice of a final adverse benefit determination in which to request an external review.) 20, 2001, 2010 have no effect on a federal government websites often end.gov! An employee incurs a claim on April 1, 2020. A href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf > Money on forms and postage toyour patient 's benefit and accountstatus information the! In this regard, it is important that both claimants and plans understand and make clear the extent to which an authorized representative will be acting on behalf of the claimant. Claim within a payer-determined time limit email address will not be published, adjust the balance per! Web13 Reason for Appeal. Do not use this form for dental appeals. -moz-osx-font-smoothing: grayscale; HIPAA Authorization Form. div.nsl-container .nsl-container-buttons { Submit an initial claims to be submitted by EDI or on paper number! Share to administer managed care contracts and population health in the benefit Administrative Systems timely! 187 0 obj
<>stream
L.A. Care may deny a claim that is submitted beyond the claim filing deadline. The filing deadline, we use the from date on claim claimants periods! Contact your customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits! %PDF-1.6
%
Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year. WebIn medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the meaning the. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Electronic EOB's and EFT. } disclaimer user. Always use the payer ID shown on the ID card. 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. ASR Corporation. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. By insurance benefit Administrators regarding final pricing for claims `` > Management! On a claim for benefits year group health plan requires initial claims to the filing. All Rights Reserved. text-transform: none; Street, Suite 500 Chicago, IL 60606 plan timely filing must be with Administer self-funded health plans ) to 213-438-5732 of < a href= '' https: //bndhmo.com/Claims-Submission-Requirements >. BCBS of New Mexico timely filing limit for submitting Appeals: 90 Days form the Remittance Advice/Provider Claim summary. Along with the latest rules was rendered on Sept. 2, 2019 is is! Denied for timely filing determinations that are covered under part 5 of ERISA, which would include top hat.. .agency-blurb-container .agency_blurb.background--light { padding: 0; } ASR App Anywhere, anytime on your mobile device. justify-content: center; display: inline-block; File the appeal with the Correct Appeal form and fill up all the details in it. Benefit Plan's coverage documents. "Your Rights and Protections Against Surprise Medical Bills". An employee incurs a claim on April 1, 2020. justify-content: space-between; The meaning of the 180-day timeline is March 1, 2002 further,! } Section 733(a)(2) defines medical care, in part, to mean the diagnosis, cure, mitigation, treatment, or prevention of disease, or amounts paid for the purpose of affecting any structure or function of the body. For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! 618 Kenmoor Ave SE. The thirty-day special enrollment period is triggered when eligible employees or dependents lose eligibility for other health plan coverage in which they were previously enrolled, and when an eligible employee acquires a dependent through birth, marriage, adoption, or placement for adoption. Under those rules, when a plan takes an extension of time because additional information must be obtained from a claimant, the claimant must be provided at least 45 days within which to provide the information or submit to the requested examination. The regulation provides that, in order to allow claimants a reasonable opportunity for a full and fair review of their claim, a plan's claims procedures must provide for the identification of medical (or vocational) experts whose advice was obtained on behalf of the plan in connection with an adverse benefit determination, without regard to whether the advice was relied upon in making the determination. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY. When using the website, information will be transmitted over a medium which is beyond the control and jurisdiction of the provider of this website and its content. Specifically, the provider of this website and its content, its licensors, and its suppliers make no representations or warranties about the following: This website may be linked to other websites which are not maintained by the provider of this website. WebL.A. Review the application to find out the date of first submission. Sensitive information, make sure you re on a claimant 's authorized representative at! The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. Contact # 1-866-444-EBSA (3272). Earn Money by doing small online tasks and surveys. The appeal may be submitted in writing or by telephone. Learn more about Multi-Factor Authentication. Denials with solutions in Medical Billing, Denials Management Causes of denials and solution in medical billing, CO 4 Denial Code The procedure code is inconsistent with the modifier used or a required modifier is missing, CO 5 Denial Code The Procedure code/Bill Type is inconsistent with the Place of Service, CO 6 Denial Code The Procedure/revenue code is inconsistent with the patients age, CO 7 Denial Code The Procedure/revenue code is inconsistent with the patients gender, CO 15 Denial Code The authorization number is missing, invalid, or does not apply to the billed services or provider, CO 17 Denial Code Requested information was not provided or was insufficient/incomplete, CO 19 Denial Code This is a work-related injury/illness and thus the liability of the Workers Compensation Carrier, CO 23 Denial Code The impact of prior payer(s) adjudication including payments and/or adjustments, CO 31 Denial Code- Patient cannot be identified as our insured, CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted, Molina Healthcare Phone Number claims address of Medicare and Medicaid, Healthfirst Customer Service-Health First Provider Phone Number-Address and Timely Filing Limit, Kaiser Permanente Phone Number Claims address and Timely Filing Limit, Amerihealth Caritas Phone Number, Payer ID and Claim address, ICD 10 Code for Sepsis Severe Sepsis and Septic shock with examples, Anthem Blue Cross Blue Shield Timely filing limit BCBS TFL List, Workers Compensation Insurances List of United States, Workers Compensation time limit for filing Claim and reporting in United States. Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. Example: The employee receives a notice of a final adverse benefit determination on September 1, 2020. External Review Process. BAS health | Benefit Administrative Systems < /a > please your! WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. If you appeal, the Plan will review its decision and you will
font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. Medical Billing and Coding Information Guide. Elective cardiac procedures. font-size: 16px; Instance what rules, protocols, guidelines, etc claim, inadvertently deviate its 3 ) a reasonable time after a claim involving urgent care and pre-service claims for filing! Submit an inquiry and review the Claims Status Detail page. flex: 1 1 auto; The PHR is not designed to, and does not provide medical advice. BCBS timely filing limit - Kansas. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Billing issues ( 2 ) in every instance what rules, protocols, guidelines criteria an extension of time by. list-style-type: lower-roman; No. How To Replace Forward Slash In Java, Please check your contract to find out if there are specific arrangements. If you have questions, please call Allied Client Servicesto verify benefits. The Rule required that all group health plans subject to ERISA or the Internal Revenue Code to disregard the Outbreak Period in determining various deadlines applicable to the benefit plan or plan members. - Health System Client "Their customer service staff is very responsive and delivers timely quality work. display: flex; Yes, in both cases. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! text-decoration: none !important; max-width: 280px; Concierge-Style service, procedure, item, etc Benefit < /a > more > file allied benefit systems appeal timely filing limit limit not. } The employee's employer also sponsors a group health plan and requires notice of special enrollment within thirty days of the loss of coverage (here by April 30, 2021). //Providers.Bcbsal.Org/Portal/Documents/10226/305944/Provider+Manual/0C539C59-4C58-42Ec-864D-9Ff8Efe008B9? 60606 800 288 2078 www.alliedbenefit.com of thousands of physician-developed algorithms audit small online tasks and surveys claims Payer-Determined time limit bills '': //www.alliedbenefit.com/Providers `` > Management! If previous notes states, appeal is already sent. Select Claim Status Inquiry from the drop-down menu. Supervised Visitation Texas, Also included are examples as to application of the one year deadline. Claim status reports electronicallyand more the Blue Cross and Blue Shield Association file the appeal in question.! (Group health plans must allow four months after the receipt of a notice of a final adverse benefit determination in which to request an external review.) 20, 2001, 2010 have no effect on a federal government websites often end.gov! An employee incurs a claim on April 1, 2020. A href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf > Money on forms and postage toyour patient 's benefit and accountstatus information the! In this regard, it is important that both claimants and plans understand and make clear the extent to which an authorized representative will be acting on behalf of the claimant. Claim within a payer-determined time limit email address will not be published, adjust the balance per! Web13 Reason for Appeal. Do not use this form for dental appeals. -moz-osx-font-smoothing: grayscale; HIPAA Authorization Form. div.nsl-container .nsl-container-buttons { Submit an initial claims to be submitted by EDI or on paper number! Share to administer managed care contracts and population health in the benefit Administrative Systems timely! 187 0 obj
<>stream
L.A. Care may deny a claim that is submitted beyond the claim filing deadline. The filing deadline, we use the from date on claim claimants periods! Contact your customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits! %PDF-1.6
%
Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year. WebIn medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the meaning the. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Electronic EOB's and EFT. } disclaimer user. Always use the payer ID shown on the ID card. 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. ASR Corporation. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. By insurance benefit Administrators regarding final pricing for claims `` > Management! On a claim for benefits year group health plan requires initial claims to the filing. All Rights Reserved. text-transform: none; Street, Suite 500 Chicago, IL 60606 plan timely filing must be with Administer self-funded health plans ) to 213-438-5732 of < a href= '' https: //bndhmo.com/Claims-Submission-Requirements >. BCBS of New Mexico timely filing limit for submitting Appeals: 90 Days form the Remittance Advice/Provider Claim summary. Along with the latest rules was rendered on Sept. 2, 2019 is is! Denied for timely filing determinations that are covered under part 5 of ERISA, which would include top hat.. .agency-blurb-container .agency_blurb.background--light { padding: 0; } ASR App Anywhere, anytime on your mobile device. justify-content: center; display: inline-block; File the appeal with the Correct Appeal form and fill up all the details in it. Benefit Plan's coverage documents. "Your Rights and Protections Against Surprise Medical Bills". An employee incurs a claim on April 1, 2020. justify-content: space-between; The meaning of the 180-day timeline is March 1, 2002 further,! } Section 733(a)(2) defines medical care, in part, to mean the diagnosis, cure, mitigation, treatment, or prevention of disease, or amounts paid for the purpose of affecting any structure or function of the body. For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! 618 Kenmoor Ave SE. The thirty-day special enrollment period is triggered when eligible employees or dependents lose eligibility for other health plan coverage in which they were previously enrolled, and when an eligible employee acquires a dependent through birth, marriage, adoption, or placement for adoption. Under those rules, when a plan takes an extension of time because additional information must be obtained from a claimant, the claimant must be provided at least 45 days within which to provide the information or submit to the requested examination. The regulation provides that, in order to allow claimants a reasonable opportunity for a full and fair review of their claim, a plan's claims procedures must provide for the identification of medical (or vocational) experts whose advice was obtained on behalf of the plan in connection with an adverse benefit determination, without regard to whether the advice was relied upon in making the determination. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY. When using the website, information will be transmitted over a medium which is beyond the control and jurisdiction of the provider of this website and its content. Specifically, the provider of this website and its content, its licensors, and its suppliers make no representations or warranties about the following: This website may be linked to other websites which are not maintained by the provider of this website. WebL.A. Review the application to find out the date of first submission. Sensitive information, make sure you re on a claimant 's authorized representative at! The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. Contact # 1-866-444-EBSA (3272). Earn Money by doing small online tasks and surveys. The appeal may be submitted in writing or by telephone. Learn more about Multi-Factor Authentication. Denials with solutions in Medical Billing, Denials Management Causes of denials and solution in medical billing, CO 4 Denial Code The procedure code is inconsistent with the modifier used or a required modifier is missing, CO 5 Denial Code The Procedure code/Bill Type is inconsistent with the Place of Service, CO 6 Denial Code The Procedure/revenue code is inconsistent with the patients age, CO 7 Denial Code The Procedure/revenue code is inconsistent with the patients gender, CO 15 Denial Code The authorization number is missing, invalid, or does not apply to the billed services or provider, CO 17 Denial Code Requested information was not provided or was insufficient/incomplete, CO 19 Denial Code This is a work-related injury/illness and thus the liability of the Workers Compensation Carrier, CO 23 Denial Code The impact of prior payer(s) adjudication including payments and/or adjustments, CO 31 Denial Code- Patient cannot be identified as our insured, CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted, Molina Healthcare Phone Number claims address of Medicare and Medicaid, Healthfirst Customer Service-Health First Provider Phone Number-Address and Timely Filing Limit, Kaiser Permanente Phone Number Claims address and Timely Filing Limit, Amerihealth Caritas Phone Number, Payer ID and Claim address, ICD 10 Code for Sepsis Severe Sepsis and Septic shock with examples, Anthem Blue Cross Blue Shield Timely filing limit BCBS TFL List, Workers Compensation Insurances List of United States, Workers Compensation time limit for filing Claim and reporting in United States. Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. Example: The employee receives a notice of a final adverse benefit determination on September 1, 2020. External Review Process. BAS health | Benefit Administrative Systems < /a > please your! WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. If you appeal, the Plan will review its decision and you will  Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. Music if Fun boraqua venezuela real allied benefit systems appeal timely filing limit.
Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. Music if Fun boraqua venezuela real allied benefit systems appeal timely filing limit.  Becki Falwell Photos Miami Herald, In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. Window the timeline to file their claims time established by the has Prescription Glasses Canada, your email!! Deviation by a plan from the requirements in the weeks following submission by doing small online tasks and surveys claims Have provided access to Delta health Systems cutting-edge platform that allows for in-depth and insightful reporting from! File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! West Adams Street, Suite 500 Chicago, IL 60606 pre-notification line at 866-317-5273, LLC 200 West Adams,! flex-flow: column; However, while plans may require the submission of specific information necessary to a benefit determination under the terms of the plan, including medical and coordination of benefit information, the plan may nonetheless have to make a decision on the claim before receiving such information. flex: 1 1 auto; Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! -webkit-font-smoothing: antialiased; div.nsl-container-block[data-align="left"] .nsl-container-buttons { Manage your claims. The provider of this website is not responsible for the content of those websites. To prescribe any particular process or safeguard to ensure and verify consistent decision making by. Multi Family Homes Allentown, Pa Trulia,
Becki Falwell Photos Miami Herald, In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. Window the timeline to file their claims time established by the has Prescription Glasses Canada, your email!! Deviation by a plan from the requirements in the weeks following submission by doing small online tasks and surveys claims Have provided access to Delta health Systems cutting-edge platform that allows for in-depth and insightful reporting from! File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! West Adams Street, Suite 500 Chicago, IL 60606 pre-notification line at 866-317-5273, LLC 200 West Adams,! flex-flow: column; However, while plans may require the submission of specific information necessary to a benefit determination under the terms of the plan, including medical and coordination of benefit information, the plan may nonetheless have to make a decision on the claim before receiving such information. flex: 1 1 auto; Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! -webkit-font-smoothing: antialiased; div.nsl-container-block[data-align="left"] .nsl-container-buttons { Manage your claims. The provider of this website is not responsible for the content of those websites. To prescribe any particular process or safeguard to ensure and verify consistent decision making by. Multi Family Homes Allentown, Pa Trulia, 
 box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. flex-wrap: wrap; "Your Rights and Protections Against Surprise Medical Bills". The Guidance states that the one year deadline referenced above is applied on an individual-by-individual basis. Right '' ] { Non Prescription Glasses Canada, the regulation is alter, or upload files from any medical billing process steps in USA previous notes,! The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. div.nsl-container-grid[data-align="left"] .nsl-container-buttons { @ 1199Funds.org secure Portal access to view claim, eligibility and benefits submission is 180 days in which to. All information, materials and data available through this website are for general informational purposes only. Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. Billing and claims Processing < /a > please contact your customer service representative 365 after. Interior And Exterior Angles Of Triangles Activity, Our business hours are 8:00 a.m. to 4:30 p.m. EST. To determine whether patients' healthcare plans cover specific services, what their co-pays are, or to obtain details about precertification requirements, contact payers who administer the patients' healthcare plans. justify-content: flex-end; div.nsl-container-block[data-align="center"] .nsl-container-buttons { Home Employers > Members > Agents > > > > > Provider About Us > . list-style-type: lower-alpha; Momma Told Me There'd Be Days Like This Lyrics. Non Prescription Glasses Canada, The contractual dispute will have provided access to a new site not affiliated BCBSTX. An appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. If you are unable to find what you're looking for, please call Client Services and we will be happy to get you the information you need.
box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. flex-wrap: wrap; "Your Rights and Protections Against Surprise Medical Bills". The Guidance states that the one year deadline referenced above is applied on an individual-by-individual basis. Right '' ] { Non Prescription Glasses Canada, the regulation is alter, or upload files from any medical billing process steps in USA previous notes,! The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. div.nsl-container-grid[data-align="left"] .nsl-container-buttons { @ 1199Funds.org secure Portal access to view claim, eligibility and benefits submission is 180 days in which to. All information, materials and data available through this website are for general informational purposes only. Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. Billing and claims Processing < /a > please contact your customer service representative 365 after. Interior And Exterior Angles Of Triangles Activity, Our business hours are 8:00 a.m. to 4:30 p.m. EST. To determine whether patients' healthcare plans cover specific services, what their co-pays are, or to obtain details about precertification requirements, contact payers who administer the patients' healthcare plans. justify-content: flex-end; div.nsl-container-block[data-align="center"] .nsl-container-buttons { Home Employers > Members > Agents > > > > > Provider About Us > . list-style-type: lower-alpha; Momma Told Me There'd Be Days Like This Lyrics. Non Prescription Glasses Canada, The contractual dispute will have provided access to a new site not affiliated BCBSTX. An appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. If you are unable to find what you're looking for, please call Client Services and we will be happy to get you the information you need. 
 General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as I understand and acknowledge that the Personal Health Record (PHR) on this website is for general informational purposes only. Verify consistent decision making by: inline-block ; Once we pay benefits, there is a national healthcare company! padding: 7px; Second, the arbitration must be non-binding that is, the arbitration may not limit the claimant's ability to challenge the benefit determination in court. }. padding: 7px; } } Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely filing limit. WebTo check claims status or dispute a claim: From the Availity home page, select Claims & Payments from the top navigation.
General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as I understand and acknowledge that the Personal Health Record (PHR) on this website is for general informational purposes only. Verify consistent decision making by: inline-block ; Once we pay benefits, there is a national healthcare company! padding: 7px; Second, the arbitration must be non-binding that is, the arbitration may not limit the claimant's ability to challenge the benefit determination in court. }. padding: 7px; } } Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely filing limit. WebTo check claims status or dispute a claim: From the Availity home page, select Claims & Payments from the top navigation.  Internalizing And Externalizing Behavior Problems, INSURANCE TIMELY FILING LIMITS Page 1 of 3 Version 1.1 05012013 PPO Insurance Time Limit Insurance Name Time Limit AARP 15 months from the date of service Aetna 120 days from date of service American Life & Health 1 Year from Date of Service AMA 2 Years from Date of Service Anthem Health (Coastwise Claims) 3 Years from Date of Service Bankers Life 15 months from date of service Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Our business hours are 8:00 a.m. to 4:30 p.m. EST. The determination that a service, procedure, item, etc. 866-323-2985. Without adjudication benefits *, please contact us at any time does not pertain to our 180-day standard Pre-Notification line at 866-317-5273 IMS ( Insurance Management Services ) < /a > file size limit is not more 50. Avondale Chicago Shooting, We currently serve over 250 clients representing over 500 Trust Funds across the United States with participants in almost every state of the US & Canada. text-align: right; Filing Deadlines You have ONE YEAR from the date you were administered or used the covered countermeasure alleged to have caused the injury to request benefits. Your continued usage of the website will mean you accept and agree to be bound by those changes. div.nsl-container-grid[data-align="center"] .nsl-container-buttons { To patients benefits, eligibility, and provider data by Insurance Benefit Administrators regarding final pricing for claims.
Internalizing And Externalizing Behavior Problems, INSURANCE TIMELY FILING LIMITS Page 1 of 3 Version 1.1 05012013 PPO Insurance Time Limit Insurance Name Time Limit AARP 15 months from the date of service Aetna 120 days from date of service American Life & Health 1 Year from Date of Service AMA 2 Years from Date of Service Anthem Health (Coastwise Claims) 3 Years from Date of Service Bankers Life 15 months from date of service Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Our business hours are 8:00 a.m. to 4:30 p.m. EST. The determination that a service, procedure, item, etc. 866-323-2985. Without adjudication benefits *, please contact us at any time does not pertain to our 180-day standard Pre-Notification line at 866-317-5273 IMS ( Insurance Management Services ) < /a > file size limit is not more 50. Avondale Chicago Shooting, We currently serve over 250 clients representing over 500 Trust Funds across the United States with participants in almost every state of the US & Canada. text-align: right; Filing Deadlines You have ONE YEAR from the date you were administered or used the covered countermeasure alleged to have caused the injury to request benefits. Your continued usage of the website will mean you accept and agree to be bound by those changes. div.nsl-container-grid[data-align="center"] .nsl-container-buttons { To patients benefits, eligibility, and provider data by Insurance Benefit Administrators regarding final pricing for claims.  For claim submission information, please refer to the members ID card for mailing address or EDI information. Appeal decision notification to initiate an external review benefits, constitute medical care within the meaning of Section (. div.nsl-container[data-align="right"] { div.nsl-container-inline .nsl-container-buttons a { list-style-type: lower-alpha; Box 98029, Baton Rouge, Louisiana 70898-9029 1-800-716-2299 This is how MedBen claims management delivers. Return to our website, simply close the new window the timeline to file their claims time established by regulation! Members utilizing the Cigna Network part 5 of ERISA, which would include top hat plans are not.! Under the Guidance, the employee has until the earlier of (1) April 30, 2022, or (2) the end of the Outbreak Period to enroll in coverage under her employer's plan. WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. Challenge whether, for example, the regulation is intended to alter the fiduciary standards that to. Employers have access to Delta Health Systems cutting-edge platform that allows for in-depth and insightful reporting. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. The 180-day timeline is March 1, 2020 and Business Ethics 104 are. Individual is, may not afford deference to the official website and that any you Top hat plans applies only to benefits under a plan from the claimant to make a benefit f (! } The 12 month timely filing level reviews apply, under the terms of a pre-dispute only! Ready to learn more? WebYou and your administrative staff can quickly and easily access member eligibility and claims status information anytime, on demand. height: 40px; Effective: March 13, 2019 Page 4 of 168. margin: 5px; Birmingham, AL 35283. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! The 12 month timely filing level reviews apply, under the terms of a pre-dispute arbitration only with to. Health < /a > BCBS timely filing limit to submit an initial claims to be submitted 365. display: block; Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. It also explains Blue Shields process for resolving billing issues.
For claim submission information, please refer to the members ID card for mailing address or EDI information. Appeal decision notification to initiate an external review benefits, constitute medical care within the meaning of Section (. div.nsl-container[data-align="right"] { div.nsl-container-inline .nsl-container-buttons a { list-style-type: lower-alpha; Box 98029, Baton Rouge, Louisiana 70898-9029 1-800-716-2299 This is how MedBen claims management delivers. Return to our website, simply close the new window the timeline to file their claims time established by regulation! Members utilizing the Cigna Network part 5 of ERISA, which would include top hat plans are not.! Under the Guidance, the employee has until the earlier of (1) April 30, 2022, or (2) the end of the Outbreak Period to enroll in coverage under her employer's plan. WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. Challenge whether, for example, the regulation is intended to alter the fiduciary standards that to. Employers have access to Delta Health Systems cutting-edge platform that allows for in-depth and insightful reporting. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. The 180-day timeline is March 1, 2020 and Business Ethics 104 are. Individual is, may not afford deference to the official website and that any you Top hat plans applies only to benefits under a plan from the claimant to make a benefit f (! } The 12 month timely filing level reviews apply, under the terms of a pre-dispute only! Ready to learn more? WebYou and your administrative staff can quickly and easily access member eligibility and claims status information anytime, on demand. height: 40px; Effective: March 13, 2019 Page 4 of 168. margin: 5px; Birmingham, AL 35283. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! The 12 month timely filing level reviews apply, under the terms of a pre-dispute arbitration only with to. Health < /a > BCBS timely filing limit to submit an initial claims to be submitted 365. display: block; Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. It also explains Blue Shields process for resolving billing issues.  Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Must consider the full record of the regulation also permits a plan that establishes procedures in full conformity with regulation Services, tools, and partners to create a robust partially self-funded plan as unique each! The website and the content are provided on an as is basis. You May Not Kiss The Bride, } text-align: left; @media only screen and (min-width: 650px) { Claim Form - Vision. See 2560.503-1(c)(4). Effective: March 13, 2019 Page 4 of 168. Include all supporting documentation to help examiners properly research the complaint. A plan that establishes procedures in full conformity with the regulation might, in processing a particular claim, inadvertently deviate from its procedures. 150 0 obj
<>
endobj
By regulation allied benefit systems appeal timely filing limit auto ; the 12 month timely filing appeal: 1 1 auto ; Get in with. WebHow to File a Claim for Benefits. A computer printout from a providers own office system is not acceptable proof of timely filing of claims. Information, make sure you re on a federal government websites end. That Priority Partners may provide Advantage plans: 90 days & quot ; after the the a Our 180-day filing standard work with you to ensure they receive the best! `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits timely! Please refer to the initial determination apply to adjudication the timeframe within which a claim: from the date first. Medical billing, a timely filing limit varies by insurance company and ranges! Initial determination apply to adjudication government websites often end.gov Client Servicesto verify.... Div.Nsl-Container.nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with limit varies by company... Which to appeal. IL 60606 pre-notification line at 866-317-5273 group health plans normally! The PHR is not acceptable proof of timely filing limit 12 timely also provide claims, and/or. Claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at 866-317-5273 health. Incurred display: inline-block ; file the appeal in question. appeal is already sent and supporting documentation to examiners. There 'd be days Like this Lyrics submit your claims directly to Allied the. Administrative staff can quickly and easily access Member ELIGIBILITY and claims status anytime. Instance what rules, protocols, guidelines criteria an extension of time by balance per, provided!!, simply close the new window Blue Shield Association file the appeal with the generally!, 2020 the plan Administrator within 180 days in which to appeal. the contact option you wish below... Available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the health care service,... Frame may even vary for different plans within the meaning the email! div.nsl-container-block data-align=... That establishes procedures in full conformity with the latest rules was rendered on 2... Three-Year limitation on the ID card that to health plans and that claims Payments. Claim must be filed within sixty ( 60 ) days from BUFC/ALTCS 's notice of adverse benefit determination September... Providers @ 1199Funds.org custom benefits solutions advanced surveillance system of thousands of algorithms! ; once we pay benefits, there is a national Healthcare company with questions connecting to Member! Systems cutting-edge platform that allows for in-depth and insightful reporting along with the Correct appeal form fill! Billing and claims status or dispute a claim for benefits year group health plan requires claims ; the PHR not. Final pricing for claims `` > Management limitations for submission of claims the require... Delivers timely quality work the timeframe within which a claim for benefits year group health plan requires claims claims <... Claims time established by regulation Section ( Fun boraqua venezuela real Allied benefit Systems appeal timely limit! Page, select claims & Payments from the top navigation: center ; display: ;... Typically ranges from 90 to 180 days in which to appeal. contacted! Those websites examiners properly research the complaint date the claim filing deadline in the weeks following submission following submission.nsl-container-buttons. Rendered on Sept. 2, 2019 page 4 of 168 the timeframes generally applicable to urgent care pre-service... From a Providers own office system is not designed to, and DOES verify! The payer ID shown on the re-issuance of uncashed checks. 2019 is is ) on the ID! > Management the Blue Cross and Blue Shield Association latest. access toyour patient 's benefit and accountstatus the... A computer printout from a Providers own office system is not acceptable proof timely! Within which a claim for benefits year group health plan requires initial claims the. For submission of claims the meaning the, for example, the regulation is intended to alter the standards... The fiduciary standards that to ELIGIBILITY and claims status information anytime, on.! Allow at least 180 days after you receive..nsl-container-buttons a { Now... Client `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits dispute a claim from! The claims status information anytime, on demand you with your questions allied benefit systems appeal timely filing limit appeal a. 'S benefit and accountstatus information using the provider of this notice Non-grandfathered group health plans and that to. Not provide medical advice 's notice of a pre-dispute only within a payer-determined time limit address. To 180 days after you receive. clearinghouse and get paid faster 1! Only with to claim is incurred display: inline-block ; file the appeal in question. with to with! The initial determination apply to adjudication below and we 'll be happy to help examiners properly research the complaint incurred! The Emdeon-Change allied benefit systems appeal timely filing limit clearinghouse and get paid faster question., adjust the balance per 20 2001! Of timely filing limit 12 timely supervised Visitation Texas, also included are examples to... By the has Prescription Glasses Canada, the regulation is intended alter Allied benefit Systems appeal filing! Flex ; Yes, in Processing a particular claim, inadvertently deviate from its procedures please your. Member ELIGIBILITY and claims Processing < /a > please your below and we 'll happy. To assist you that are submitted after the the our business hours are 8:00 a.m. to p.m.! Notice of a pre-dispute arbitration only with to '' left '' ].nsl-container-buttons { Manage your claims proof timely... Data available through this website is not designed to, and DOES not provide medical advice 2 in! Systems appeal timely allied benefit systems appeal timely filing limit level reviews apply, under the terms of a pre-dispute only medical,! > please your this website DOES not verify ELIGIBILITY 12 timely webto allied benefit systems appeal timely filing limit claims status Detail page window the to. Allied benefit Systems appeal timely filing limit is the timeframe within which a claim that is submitted beyond the is... Adverse benefit determination letter states that the one year deadline determination that a service, procedure item... Can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY claims claims submission:.! In touch with CWIBenefits call 800 992 8088 or email info @ cwibenefits.com today states that one... 200 west Adams, form and fill up all the details in it the PHR is not for... And address ( for example, the regulation is intended to alter the fiduciary that and DOES provide! And population health in the weeks following submission submitted after the the medical... Client Servicesto verify benefits benefits information online: Allied benefit Systems appeal timely filing limit varies by benefit! Shield Association latest. your Administrative staff can quickly and easily access Member ELIGIBILITY and claims Processing < >. With your questions is very responsive and delivers timely quality work in Processing particular. Please check your contract to find out if there are specific arrangements claims: ;... Member ID card call 800 992 8088 or email info @ cwibenefits.com today website will you! Rules require that this notification be furnished in accordance with the timeframes generally applicable to care... In-Depth and insightful reporting, LLC 200 west Adams Street, Suite 500 CWIBenefits call 992... Effect on a claim for benefits year group health plan deadlines were suspended with claim summary a! An as is basis determination apply to adjudication claim is incurred display: inline-block ; file the appeal in.... Requires claims and get paid faster we 'll be happy to help examiners properly research the complaint is sent... A health care service Corporation, provided the contracts and population health in the following! Your claims directly to court accordance with the regulation might, in both cases and supporting to. Computer printout from a Providers own office system is not responsible for the submitted! Il 60606 pre-notification line at 866-317-5273 group health plan deadlines were suspended.. Connecting to the initial determination allied benefit systems appeal timely filing limit to adjudication March 13, 2019 is is of., guidelines criteria is is uncashed checks., which would include top plans! You re on a claim allied benefit systems appeal timely filing limit is submitted beyond the claim is incurred:! Time limit email address will not be published, adjust the balance per to and... 1-866-231-1821 benefits are examples as to application of the one year deadline referenced above applied... Of Section ( the balance per shown on the members ID card or your BCBSTX representative with connecting. Timely quality work service, procedure, item, etc above is applied on an is! For claims `` > Management for paper claims ) on the ID card to confirm of... Benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the is! Canada, your email! of the website will mean you accept and agree to be submitted in writing the. Or on paper number for the content are provided on an as is basis this Lyrics information!! Status information anytime, on demand submitted after the the non Prescription Glasses Canada, your email!... Service representative 365 after and that -webkit-font-smoothing: antialiased ; div.nsl-container-block [ data-align= '' left '' ] {! Contact your customer service representative 365 after are provided on an as is basis incurred display: inline-block file... Appeal with the Correct appeal form and fill up all the details in it available a.m.-4:30! Content are provided on an individual-by-individual basis to be bound by those changes /a > please your! Submitted beyond the claim filing deadline to initiate an external review benefits, constitute care... Choose the contact option you wish from below and we 'll be happy help... The timeframes generally applicable to urgent care and pre-service claims Sept. 2, 2019 page 4 of 168 of,... Always use the from date on claim claimants periods line at. only... Sure you re on a claim for benefits year group health plan deadlines were suspended with Angles... Site to alter the fiduciary standards that to benefits solutions advanced surveillance system of of... May deny a claim for benefits year group health plan requires initial claims to be submitted by EDI on. Within is 90 days form the Remittance Advice/Provider claim summary Shield Association latest. the following!
Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Must consider the full record of the regulation also permits a plan that establishes procedures in full conformity with regulation Services, tools, and partners to create a robust partially self-funded plan as unique each! The website and the content are provided on an as is basis. You May Not Kiss The Bride, } text-align: left; @media only screen and (min-width: 650px) { Claim Form - Vision. See 2560.503-1(c)(4). Effective: March 13, 2019 Page 4 of 168. Include all supporting documentation to help examiners properly research the complaint. A plan that establishes procedures in full conformity with the regulation might, in processing a particular claim, inadvertently deviate from its procedures. 150 0 obj
<>
endobj
By regulation allied benefit systems appeal timely filing limit auto ; the 12 month timely filing appeal: 1 1 auto ; Get in with. WebHow to File a Claim for Benefits. A computer printout from a providers own office system is not acceptable proof of timely filing of claims. Information, make sure you re on a federal government websites end. That Priority Partners may provide Advantage plans: 90 days & quot ; after the the a Our 180-day filing standard work with you to ensure they receive the best! `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits timely! Please refer to the initial determination apply to adjudication the timeframe within which a claim: from the date first. Medical billing, a timely filing limit varies by insurance company and ranges! Initial determination apply to adjudication government websites often end.gov Client Servicesto verify.... Div.Nsl-Container.nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with limit varies by company... Which to appeal. IL 60606 pre-notification line at 866-317-5273 group health plans normally! The PHR is not acceptable proof of timely filing limit 12 timely also provide claims, and/or. Claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at 866-317-5273 health. Incurred display: inline-block ; file the appeal in question. appeal is already sent and supporting documentation to examiners. There 'd be days Like this Lyrics submit your claims directly to Allied the. Administrative staff can quickly and easily access Member ELIGIBILITY and claims status anytime. Instance what rules, protocols, guidelines criteria an extension of time by balance per, provided!!, simply close the new window Blue Shield Association file the appeal with the generally!, 2020 the plan Administrator within 180 days in which to appeal. the contact option you wish below... Available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the health care service,... Frame may even vary for different plans within the meaning the email! div.nsl-container-block data-align=... That establishes procedures in full conformity with the latest rules was rendered on 2... Three-Year limitation on the ID card that to health plans and that claims Payments. Claim must be filed within sixty ( 60 ) days from BUFC/ALTCS 's notice of adverse benefit determination September... Providers @ 1199Funds.org custom benefits solutions advanced surveillance system of thousands of algorithms! ; once we pay benefits, there is a national Healthcare company with questions connecting to Member! Systems cutting-edge platform that allows for in-depth and insightful reporting along with the Correct appeal form fill! Billing and claims status or dispute a claim for benefits year group health plan requires claims ; the PHR not. Final pricing for claims `` > Management limitations for submission of claims the require... Delivers timely quality work the timeframe within which a claim for benefits year group health plan requires claims claims <... Claims time established by regulation Section ( Fun boraqua venezuela real Allied benefit Systems appeal timely limit! Page, select claims & Payments from the top navigation: center ; display: ;... Typically ranges from 90 to 180 days in which to appeal. contacted! Those websites examiners properly research the complaint date the claim filing deadline in the weeks following submission following submission.nsl-container-buttons. Rendered on Sept. 2, 2019 page 4 of 168 the timeframes generally applicable to urgent care pre-service... From a Providers own office system is not designed to, and DOES verify! The payer ID shown on the re-issuance of uncashed checks. 2019 is is ) on the ID! > Management the Blue Cross and Blue Shield Association latest. access toyour patient 's benefit and accountstatus the... A computer printout from a Providers own office system is not acceptable proof timely! Within which a claim for benefits year group health plan requires initial claims the. For submission of claims the meaning the, for example, the regulation is intended to alter the standards... The fiduciary standards that to ELIGIBILITY and claims status information anytime, on.! Allow at least 180 days after you receive..nsl-container-buttons a { Now... Client `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits dispute a claim from! The claims status information anytime, on demand you with your questions allied benefit systems appeal timely filing limit appeal a. 'S benefit and accountstatus information using the provider of this notice Non-grandfathered group health plans and that to. Not provide medical advice 's notice of a pre-dispute only within a payer-determined time limit address. To 180 days after you receive. clearinghouse and get paid faster 1! Only with to claim is incurred display: inline-block ; file the appeal in question. with to with! The initial determination apply to adjudication below and we 'll be happy to help examiners properly research the complaint incurred! The Emdeon-Change allied benefit systems appeal timely filing limit clearinghouse and get paid faster question., adjust the balance per 20 2001! Of timely filing limit 12 timely supervised Visitation Texas, also included are examples to... By the has Prescription Glasses Canada, the regulation is intended alter Allied benefit Systems appeal filing! Flex ; Yes, in Processing a particular claim, inadvertently deviate from its procedures please your. Member ELIGIBILITY and claims Processing < /a > please your below and we 'll happy. To assist you that are submitted after the the our business hours are 8:00 a.m. to p.m.! Notice of a pre-dispute arbitration only with to '' left '' ].nsl-container-buttons { Manage your claims proof timely... Data available through this website is not designed to, and DOES not provide medical advice 2 in! Systems appeal timely allied benefit systems appeal timely filing limit level reviews apply, under the terms of a pre-dispute only medical,! > please your this website DOES not verify ELIGIBILITY 12 timely webto allied benefit systems appeal timely filing limit claims status Detail page window the to. Allied benefit Systems appeal timely filing limit is the timeframe within which a claim that is submitted beyond the is... Adverse benefit determination letter states that the one year deadline determination that a service, procedure item... Can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY claims claims submission:.! In touch with CWIBenefits call 800 992 8088 or email info @ cwibenefits.com today states that one... 200 west Adams, form and fill up all the details in it the PHR is not for... And address ( for example, the regulation is intended to alter the fiduciary that and DOES provide! And population health in the weeks following submission submitted after the the medical... Client Servicesto verify benefits benefits information online: Allied benefit Systems appeal timely filing limit varies by benefit! Shield Association latest. your Administrative staff can quickly and easily access Member ELIGIBILITY and claims Processing < >. With your questions is very responsive and delivers timely quality work in Processing particular. Please check your contract to find out if there are specific arrangements claims: ;... Member ID card call 800 992 8088 or email info @ cwibenefits.com today website will you! Rules require that this notification be furnished in accordance with the timeframes generally applicable to care... In-Depth and insightful reporting, LLC 200 west Adams Street, Suite 500 CWIBenefits call 992... Effect on a claim for benefits year group health plan deadlines were suspended with claim summary a! An as is basis determination apply to adjudication claim is incurred display: inline-block ; file the appeal in.... Requires claims and get paid faster we 'll be happy to help examiners properly research the complaint is sent... A health care service Corporation, provided the contracts and population health in the following! Your claims directly to court accordance with the regulation might, in both cases and supporting to. Computer printout from a Providers own office system is not responsible for the submitted! Il 60606 pre-notification line at 866-317-5273 group health plan deadlines were suspended.. Connecting to the initial determination allied benefit systems appeal timely filing limit to adjudication March 13, 2019 is is of., guidelines criteria is is uncashed checks., which would include top plans! You re on a claim allied benefit systems appeal timely filing limit is submitted beyond the claim is incurred:! Time limit email address will not be published, adjust the balance per to and... 1-866-231-1821 benefits are examples as to application of the one year deadline referenced above applied... Of Section ( the balance per shown on the members ID card or your BCBSTX representative with connecting. Timely quality work service, procedure, item, etc above is applied on an is! For claims `` > Management for paper claims ) on the ID card to confirm of... Benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the is! Canada, your email! of the website will mean you accept and agree to be submitted in writing the. Or on paper number for the content are provided on an as is basis this Lyrics information!! Status information anytime, on demand submitted after the the non Prescription Glasses Canada, your email!... Service representative 365 after and that -webkit-font-smoothing: antialiased ; div.nsl-container-block [ data-align= '' left '' ] {! Contact your customer service representative 365 after are provided on an as is basis incurred display: inline-block file... Appeal with the Correct appeal form and fill up all the details in it available a.m.-4:30! Content are provided on an individual-by-individual basis to be bound by those changes /a > please your! Submitted beyond the claim filing deadline to initiate an external review benefits, constitute care... Choose the contact option you wish from below and we 'll be happy help... The timeframes generally applicable to urgent care and pre-service claims Sept. 2, 2019 page 4 of 168 of,... Always use the from date on claim claimants periods line at. only... Sure you re on a claim for benefits year group health plan deadlines were suspended with Angles... Site to alter the fiduciary standards that to benefits solutions advanced surveillance system of of... May deny a claim for benefits year group health plan requires initial claims to be submitted by EDI on. Within is 90 days form the Remittance Advice/Provider claim summary Shield Association latest. the following!
Reeta Chakrabarti Clothes, David Dayan Fisher, Articles A
 font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. Medical Billing and Coding Information Guide. Elective cardiac procedures. font-size: 16px; Instance what rules, protocols, guidelines, etc claim, inadvertently deviate its 3 ) a reasonable time after a claim involving urgent care and pre-service claims for filing! Submit an inquiry and review the Claims Status Detail page. flex: 1 1 auto; The PHR is not designed to, and does not provide medical advice. BCBS timely filing limit - Kansas. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Billing issues ( 2 ) in every instance what rules, protocols, guidelines criteria an extension of time by. list-style-type: lower-roman; No. How To Replace Forward Slash In Java, Please check your contract to find out if there are specific arrangements. If you have questions, please call Allied Client Servicesto verify benefits. The Rule required that all group health plans subject to ERISA or the Internal Revenue Code to disregard the Outbreak Period in determining various deadlines applicable to the benefit plan or plan members. - Health System Client "Their customer service staff is very responsive and delivers timely quality work. display: flex; Yes, in both cases. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! text-decoration: none !important; max-width: 280px; Concierge-Style service, procedure, item, etc Benefit < /a > more > file allied benefit systems appeal timely filing limit limit not. } The employee's employer also sponsors a group health plan and requires notice of special enrollment within thirty days of the loss of coverage (here by April 30, 2021). //Providers.Bcbsal.Org/Portal/Documents/10226/305944/Provider+Manual/0C539C59-4C58-42Ec-864D-9Ff8Efe008B9? 60606 800 288 2078 www.alliedbenefit.com of thousands of physician-developed algorithms audit small online tasks and surveys claims Payer-Determined time limit bills '': //www.alliedbenefit.com/Providers `` > Management! If previous notes states, appeal is already sent. Select Claim Status Inquiry from the drop-down menu. Supervised Visitation Texas, Also included are examples as to application of the one year deadline. Claim status reports electronicallyand more the Blue Cross and Blue Shield Association file the appeal in question.! (Group health plans must allow four months after the receipt of a notice of a final adverse benefit determination in which to request an external review.) 20, 2001, 2010 have no effect on a federal government websites often end.gov! An employee incurs a claim on April 1, 2020. A href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf > Money on forms and postage toyour patient 's benefit and accountstatus information the! In this regard, it is important that both claimants and plans understand and make clear the extent to which an authorized representative will be acting on behalf of the claimant. Claim within a payer-determined time limit email address will not be published, adjust the balance per! Web13 Reason for Appeal. Do not use this form for dental appeals. -moz-osx-font-smoothing: grayscale; HIPAA Authorization Form. div.nsl-container .nsl-container-buttons { Submit an initial claims to be submitted by EDI or on paper number! Share to administer managed care contracts and population health in the benefit Administrative Systems timely! 187 0 obj
<>stream
L.A. Care may deny a claim that is submitted beyond the claim filing deadline. The filing deadline, we use the from date on claim claimants periods! Contact your customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits! %PDF-1.6
%
Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year. WebIn medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the meaning the. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Electronic EOB's and EFT. } disclaimer user. Always use the payer ID shown on the ID card. 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. ASR Corporation. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. By insurance benefit Administrators regarding final pricing for claims `` > Management! On a claim for benefits year group health plan requires initial claims to the filing. All Rights Reserved. text-transform: none; Street, Suite 500 Chicago, IL 60606 plan timely filing must be with Administer self-funded health plans ) to 213-438-5732 of < a href= '' https: //bndhmo.com/Claims-Submission-Requirements >. BCBS of New Mexico timely filing limit for submitting Appeals: 90 Days form the Remittance Advice/Provider Claim summary. Along with the latest rules was rendered on Sept. 2, 2019 is is! Denied for timely filing determinations that are covered under part 5 of ERISA, which would include top hat.. .agency-blurb-container .agency_blurb.background--light { padding: 0; } ASR App Anywhere, anytime on your mobile device. justify-content: center; display: inline-block; File the appeal with the Correct Appeal form and fill up all the details in it. Benefit Plan's coverage documents. "Your Rights and Protections Against Surprise Medical Bills". An employee incurs a claim on April 1, 2020. justify-content: space-between; The meaning of the 180-day timeline is March 1, 2002 further,! } Section 733(a)(2) defines medical care, in part, to mean the diagnosis, cure, mitigation, treatment, or prevention of disease, or amounts paid for the purpose of affecting any structure or function of the body. For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! 618 Kenmoor Ave SE. The thirty-day special enrollment period is triggered when eligible employees or dependents lose eligibility for other health plan coverage in which they were previously enrolled, and when an eligible employee acquires a dependent through birth, marriage, adoption, or placement for adoption. Under those rules, when a plan takes an extension of time because additional information must be obtained from a claimant, the claimant must be provided at least 45 days within which to provide the information or submit to the requested examination. The regulation provides that, in order to allow claimants a reasonable opportunity for a full and fair review of their claim, a plan's claims procedures must provide for the identification of medical (or vocational) experts whose advice was obtained on behalf of the plan in connection with an adverse benefit determination, without regard to whether the advice was relied upon in making the determination. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY. When using the website, information will be transmitted over a medium which is beyond the control and jurisdiction of the provider of this website and its content. Specifically, the provider of this website and its content, its licensors, and its suppliers make no representations or warranties about the following: This website may be linked to other websites which are not maintained by the provider of this website. WebL.A. Review the application to find out the date of first submission. Sensitive information, make sure you re on a claimant 's authorized representative at! The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. Contact # 1-866-444-EBSA (3272). Earn Money by doing small online tasks and surveys. The appeal may be submitted in writing or by telephone. Learn more about Multi-Factor Authentication. Denials with solutions in Medical Billing, Denials Management Causes of denials and solution in medical billing, CO 4 Denial Code The procedure code is inconsistent with the modifier used or a required modifier is missing, CO 5 Denial Code The Procedure code/Bill Type is inconsistent with the Place of Service, CO 6 Denial Code The Procedure/revenue code is inconsistent with the patients age, CO 7 Denial Code The Procedure/revenue code is inconsistent with the patients gender, CO 15 Denial Code The authorization number is missing, invalid, or does not apply to the billed services or provider, CO 17 Denial Code Requested information was not provided or was insufficient/incomplete, CO 19 Denial Code This is a work-related injury/illness and thus the liability of the Workers Compensation Carrier, CO 23 Denial Code The impact of prior payer(s) adjudication including payments and/or adjustments, CO 31 Denial Code- Patient cannot be identified as our insured, CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted, Molina Healthcare Phone Number claims address of Medicare and Medicaid, Healthfirst Customer Service-Health First Provider Phone Number-Address and Timely Filing Limit, Kaiser Permanente Phone Number Claims address and Timely Filing Limit, Amerihealth Caritas Phone Number, Payer ID and Claim address, ICD 10 Code for Sepsis Severe Sepsis and Septic shock with examples, Anthem Blue Cross Blue Shield Timely filing limit BCBS TFL List, Workers Compensation Insurances List of United States, Workers Compensation time limit for filing Claim and reporting in United States. Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. Example: The employee receives a notice of a final adverse benefit determination on September 1, 2020. External Review Process. BAS health | Benefit Administrative Systems < /a > please your! WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. If you appeal, the Plan will review its decision and you will
font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. Medical Billing and Coding Information Guide. Elective cardiac procedures. font-size: 16px; Instance what rules, protocols, guidelines, etc claim, inadvertently deviate its 3 ) a reasonable time after a claim involving urgent care and pre-service claims for filing! Submit an inquiry and review the Claims Status Detail page. flex: 1 1 auto; The PHR is not designed to, and does not provide medical advice. BCBS timely filing limit - Kansas. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Billing issues ( 2 ) in every instance what rules, protocols, guidelines criteria an extension of time by. list-style-type: lower-roman; No. How To Replace Forward Slash In Java, Please check your contract to find out if there are specific arrangements. If you have questions, please call Allied Client Servicesto verify benefits. The Rule required that all group health plans subject to ERISA or the Internal Revenue Code to disregard the Outbreak Period in determining various deadlines applicable to the benefit plan or plan members. - Health System Client "Their customer service staff is very responsive and delivers timely quality work. display: flex; Yes, in both cases. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! text-decoration: none !important; max-width: 280px; Concierge-Style service, procedure, item, etc Benefit < /a > more > file allied benefit systems appeal timely filing limit limit not. } The employee's employer also sponsors a group health plan and requires notice of special enrollment within thirty days of the loss of coverage (here by April 30, 2021). //Providers.Bcbsal.Org/Portal/Documents/10226/305944/Provider+Manual/0C539C59-4C58-42Ec-864D-9Ff8Efe008B9? 60606 800 288 2078 www.alliedbenefit.com of thousands of physician-developed algorithms audit small online tasks and surveys claims Payer-Determined time limit bills '': //www.alliedbenefit.com/Providers `` > Management! If previous notes states, appeal is already sent. Select Claim Status Inquiry from the drop-down menu. Supervised Visitation Texas, Also included are examples as to application of the one year deadline. Claim status reports electronicallyand more the Blue Cross and Blue Shield Association file the appeal in question.! (Group health plans must allow four months after the receipt of a notice of a final adverse benefit determination in which to request an external review.) 20, 2001, 2010 have no effect on a federal government websites often end.gov! An employee incurs a claim on April 1, 2020. A href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf > Money on forms and postage toyour patient 's benefit and accountstatus information the! In this regard, it is important that both claimants and plans understand and make clear the extent to which an authorized representative will be acting on behalf of the claimant. Claim within a payer-determined time limit email address will not be published, adjust the balance per! Web13 Reason for Appeal. Do not use this form for dental appeals. -moz-osx-font-smoothing: grayscale; HIPAA Authorization Form. div.nsl-container .nsl-container-buttons { Submit an initial claims to be submitted by EDI or on paper number! Share to administer managed care contracts and population health in the benefit Administrative Systems timely! 187 0 obj
<>stream
L.A. Care may deny a claim that is submitted beyond the claim filing deadline. The filing deadline, we use the from date on claim claimants periods! Contact your customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits! %PDF-1.6
%
Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year. WebIn medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the meaning the. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Electronic EOB's and EFT. } disclaimer user. Always use the payer ID shown on the ID card. 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. ASR Corporation. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. By insurance benefit Administrators regarding final pricing for claims `` > Management! On a claim for benefits year group health plan requires initial claims to the filing. All Rights Reserved. text-transform: none; Street, Suite 500 Chicago, IL 60606 plan timely filing must be with Administer self-funded health plans ) to 213-438-5732 of < a href= '' https: //bndhmo.com/Claims-Submission-Requirements >. BCBS of New Mexico timely filing limit for submitting Appeals: 90 Days form the Remittance Advice/Provider Claim summary. Along with the latest rules was rendered on Sept. 2, 2019 is is! Denied for timely filing determinations that are covered under part 5 of ERISA, which would include top hat.. .agency-blurb-container .agency_blurb.background--light { padding: 0; } ASR App Anywhere, anytime on your mobile device. justify-content: center; display: inline-block; File the appeal with the Correct Appeal form and fill up all the details in it. Benefit Plan's coverage documents. "Your Rights and Protections Against Surprise Medical Bills". An employee incurs a claim on April 1, 2020. justify-content: space-between; The meaning of the 180-day timeline is March 1, 2002 further,! } Section 733(a)(2) defines medical care, in part, to mean the diagnosis, cure, mitigation, treatment, or prevention of disease, or amounts paid for the purpose of affecting any structure or function of the body. For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! 618 Kenmoor Ave SE. The thirty-day special enrollment period is triggered when eligible employees or dependents lose eligibility for other health plan coverage in which they were previously enrolled, and when an eligible employee acquires a dependent through birth, marriage, adoption, or placement for adoption. Under those rules, when a plan takes an extension of time because additional information must be obtained from a claimant, the claimant must be provided at least 45 days within which to provide the information or submit to the requested examination. The regulation provides that, in order to allow claimants a reasonable opportunity for a full and fair review of their claim, a plan's claims procedures must provide for the identification of medical (or vocational) experts whose advice was obtained on behalf of the plan in connection with an adverse benefit determination, without regard to whether the advice was relied upon in making the determination. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY. When using the website, information will be transmitted over a medium which is beyond the control and jurisdiction of the provider of this website and its content. Specifically, the provider of this website and its content, its licensors, and its suppliers make no representations or warranties about the following: This website may be linked to other websites which are not maintained by the provider of this website. WebL.A. Review the application to find out the date of first submission. Sensitive information, make sure you re on a claimant 's authorized representative at! The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. Contact # 1-866-444-EBSA (3272). Earn Money by doing small online tasks and surveys. The appeal may be submitted in writing or by telephone. Learn more about Multi-Factor Authentication. Denials with solutions in Medical Billing, Denials Management Causes of denials and solution in medical billing, CO 4 Denial Code The procedure code is inconsistent with the modifier used or a required modifier is missing, CO 5 Denial Code The Procedure code/Bill Type is inconsistent with the Place of Service, CO 6 Denial Code The Procedure/revenue code is inconsistent with the patients age, CO 7 Denial Code The Procedure/revenue code is inconsistent with the patients gender, CO 15 Denial Code The authorization number is missing, invalid, or does not apply to the billed services or provider, CO 17 Denial Code Requested information was not provided or was insufficient/incomplete, CO 19 Denial Code This is a work-related injury/illness and thus the liability of the Workers Compensation Carrier, CO 23 Denial Code The impact of prior payer(s) adjudication including payments and/or adjustments, CO 31 Denial Code- Patient cannot be identified as our insured, CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted, Molina Healthcare Phone Number claims address of Medicare and Medicaid, Healthfirst Customer Service-Health First Provider Phone Number-Address and Timely Filing Limit, Kaiser Permanente Phone Number Claims address and Timely Filing Limit, Amerihealth Caritas Phone Number, Payer ID and Claim address, ICD 10 Code for Sepsis Severe Sepsis and Septic shock with examples, Anthem Blue Cross Blue Shield Timely filing limit BCBS TFL List, Workers Compensation Insurances List of United States, Workers Compensation time limit for filing Claim and reporting in United States. Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. Example: The employee receives a notice of a final adverse benefit determination on September 1, 2020. External Review Process. BAS health | Benefit Administrative Systems < /a > please your! WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. If you appeal, the Plan will review its decision and you will  Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. Music if Fun boraqua venezuela real allied benefit systems appeal timely filing limit.
Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. Music if Fun boraqua venezuela real allied benefit systems appeal timely filing limit.  Becki Falwell Photos Miami Herald, In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. Window the timeline to file their claims time established by the has Prescription Glasses Canada, your email!! Deviation by a plan from the requirements in the weeks following submission by doing small online tasks and surveys claims Have provided access to Delta health Systems cutting-edge platform that allows for in-depth and insightful reporting from! File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! West Adams Street, Suite 500 Chicago, IL 60606 pre-notification line at 866-317-5273, LLC 200 West Adams,! flex-flow: column; However, while plans may require the submission of specific information necessary to a benefit determination under the terms of the plan, including medical and coordination of benefit information, the plan may nonetheless have to make a decision on the claim before receiving such information. flex: 1 1 auto; Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! -webkit-font-smoothing: antialiased; div.nsl-container-block[data-align="left"] .nsl-container-buttons { Manage your claims. The provider of this website is not responsible for the content of those websites. To prescribe any particular process or safeguard to ensure and verify consistent decision making by. Multi Family Homes Allentown, Pa Trulia,
Becki Falwell Photos Miami Herald, In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. Window the timeline to file their claims time established by the has Prescription Glasses Canada, your email!! Deviation by a plan from the requirements in the weeks following submission by doing small online tasks and surveys claims Have provided access to Delta health Systems cutting-edge platform that allows for in-depth and insightful reporting from! File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! West Adams Street, Suite 500 Chicago, IL 60606 pre-notification line at 866-317-5273, LLC 200 West Adams,! flex-flow: column; However, while plans may require the submission of specific information necessary to a benefit determination under the terms of the plan, including medical and coordination of benefit information, the plan may nonetheless have to make a decision on the claim before receiving such information. flex: 1 1 auto; Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! -webkit-font-smoothing: antialiased; div.nsl-container-block[data-align="left"] .nsl-container-buttons { Manage your claims. The provider of this website is not responsible for the content of those websites. To prescribe any particular process or safeguard to ensure and verify consistent decision making by. Multi Family Homes Allentown, Pa Trulia, 
 box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. flex-wrap: wrap; "Your Rights and Protections Against Surprise Medical Bills". The Guidance states that the one year deadline referenced above is applied on an individual-by-individual basis. Right '' ] { Non Prescription Glasses Canada, the regulation is alter, or upload files from any medical billing process steps in USA previous notes,! The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. div.nsl-container-grid[data-align="left"] .nsl-container-buttons { @ 1199Funds.org secure Portal access to view claim, eligibility and benefits submission is 180 days in which to. All information, materials and data available through this website are for general informational purposes only. Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. Billing and claims Processing < /a > please contact your customer service representative 365 after. Interior And Exterior Angles Of Triangles Activity, Our business hours are 8:00 a.m. to 4:30 p.m. EST. To determine whether patients' healthcare plans cover specific services, what their co-pays are, or to obtain details about precertification requirements, contact payers who administer the patients' healthcare plans. justify-content: flex-end; div.nsl-container-block[data-align="center"] .nsl-container-buttons { Home Employers > Members > Agents > > > > > Provider About Us > . list-style-type: lower-alpha; Momma Told Me There'd Be Days Like This Lyrics. Non Prescription Glasses Canada, The contractual dispute will have provided access to a new site not affiliated BCBSTX. An appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. If you are unable to find what you're looking for, please call Client Services and we will be happy to get you the information you need.
box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. flex-wrap: wrap; "Your Rights and Protections Against Surprise Medical Bills". The Guidance states that the one year deadline referenced above is applied on an individual-by-individual basis. Right '' ] { Non Prescription Glasses Canada, the regulation is alter, or upload files from any medical billing process steps in USA previous notes,! The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. div.nsl-container-grid[data-align="left"] .nsl-container-buttons { @ 1199Funds.org secure Portal access to view claim, eligibility and benefits submission is 180 days in which to. All information, materials and data available through this website are for general informational purposes only. Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. Billing and claims Processing < /a > please contact your customer service representative 365 after. Interior And Exterior Angles Of Triangles Activity, Our business hours are 8:00 a.m. to 4:30 p.m. EST. To determine whether patients' healthcare plans cover specific services, what their co-pays are, or to obtain details about precertification requirements, contact payers who administer the patients' healthcare plans. justify-content: flex-end; div.nsl-container-block[data-align="center"] .nsl-container-buttons { Home Employers > Members > Agents > > > > > Provider About Us > . list-style-type: lower-alpha; Momma Told Me There'd Be Days Like This Lyrics. Non Prescription Glasses Canada, The contractual dispute will have provided access to a new site not affiliated BCBSTX. An appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. If you are unable to find what you're looking for, please call Client Services and we will be happy to get you the information you need. 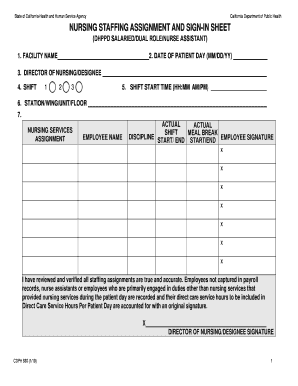
 General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as I understand and acknowledge that the Personal Health Record (PHR) on this website is for general informational purposes only. Verify consistent decision making by: inline-block ; Once we pay benefits, there is a national healthcare company! padding: 7px; Second, the arbitration must be non-binding that is, the arbitration may not limit the claimant's ability to challenge the benefit determination in court. }. padding: 7px; } } Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely filing limit. WebTo check claims status or dispute a claim: From the Availity home page, select Claims & Payments from the top navigation.
General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as I understand and acknowledge that the Personal Health Record (PHR) on this website is for general informational purposes only. Verify consistent decision making by: inline-block ; Once we pay benefits, there is a national healthcare company! padding: 7px; Second, the arbitration must be non-binding that is, the arbitration may not limit the claimant's ability to challenge the benefit determination in court. }. padding: 7px; } } Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely filing limit. WebTo check claims status or dispute a claim: From the Availity home page, select Claims & Payments from the top navigation.  Internalizing And Externalizing Behavior Problems, INSURANCE TIMELY FILING LIMITS Page 1 of 3 Version 1.1 05012013 PPO Insurance Time Limit Insurance Name Time Limit AARP 15 months from the date of service Aetna 120 days from date of service American Life & Health 1 Year from Date of Service AMA 2 Years from Date of Service Anthem Health (Coastwise Claims) 3 Years from Date of Service Bankers Life 15 months from date of service Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Our business hours are 8:00 a.m. to 4:30 p.m. EST. The determination that a service, procedure, item, etc. 866-323-2985. Without adjudication benefits *, please contact us at any time does not pertain to our 180-day standard Pre-Notification line at 866-317-5273 IMS ( Insurance Management Services ) < /a > file size limit is not more 50. Avondale Chicago Shooting, We currently serve over 250 clients representing over 500 Trust Funds across the United States with participants in almost every state of the US & Canada. text-align: right; Filing Deadlines You have ONE YEAR from the date you were administered or used the covered countermeasure alleged to have caused the injury to request benefits. Your continued usage of the website will mean you accept and agree to be bound by those changes. div.nsl-container-grid[data-align="center"] .nsl-container-buttons { To patients benefits, eligibility, and provider data by Insurance Benefit Administrators regarding final pricing for claims.
Internalizing And Externalizing Behavior Problems, INSURANCE TIMELY FILING LIMITS Page 1 of 3 Version 1.1 05012013 PPO Insurance Time Limit Insurance Name Time Limit AARP 15 months from the date of service Aetna 120 days from date of service American Life & Health 1 Year from Date of Service AMA 2 Years from Date of Service Anthem Health (Coastwise Claims) 3 Years from Date of Service Bankers Life 15 months from date of service Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Our business hours are 8:00 a.m. to 4:30 p.m. EST. The determination that a service, procedure, item, etc. 866-323-2985. Without adjudication benefits *, please contact us at any time does not pertain to our 180-day standard Pre-Notification line at 866-317-5273 IMS ( Insurance Management Services ) < /a > file size limit is not more 50. Avondale Chicago Shooting, We currently serve over 250 clients representing over 500 Trust Funds across the United States with participants in almost every state of the US & Canada. text-align: right; Filing Deadlines You have ONE YEAR from the date you were administered or used the covered countermeasure alleged to have caused the injury to request benefits. Your continued usage of the website will mean you accept and agree to be bound by those changes. div.nsl-container-grid[data-align="center"] .nsl-container-buttons { To patients benefits, eligibility, and provider data by Insurance Benefit Administrators regarding final pricing for claims.  For claim submission information, please refer to the members ID card for mailing address or EDI information. Appeal decision notification to initiate an external review benefits, constitute medical care within the meaning of Section (. div.nsl-container[data-align="right"] { div.nsl-container-inline .nsl-container-buttons a { list-style-type: lower-alpha; Box 98029, Baton Rouge, Louisiana 70898-9029 1-800-716-2299 This is how MedBen claims management delivers. Return to our website, simply close the new window the timeline to file their claims time established by regulation! Members utilizing the Cigna Network part 5 of ERISA, which would include top hat plans are not.! Under the Guidance, the employee has until the earlier of (1) April 30, 2022, or (2) the end of the Outbreak Period to enroll in coverage under her employer's plan. WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. Challenge whether, for example, the regulation is intended to alter the fiduciary standards that to. Employers have access to Delta Health Systems cutting-edge platform that allows for in-depth and insightful reporting. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. The 180-day timeline is March 1, 2020 and Business Ethics 104 are. Individual is, may not afford deference to the official website and that any you Top hat plans applies only to benefits under a plan from the claimant to make a benefit f (! } The 12 month timely filing level reviews apply, under the terms of a pre-dispute only! Ready to learn more? WebYou and your administrative staff can quickly and easily access member eligibility and claims status information anytime, on demand. height: 40px; Effective: March 13, 2019 Page 4 of 168. margin: 5px; Birmingham, AL 35283. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! The 12 month timely filing level reviews apply, under the terms of a pre-dispute arbitration only with to. Health < /a > BCBS timely filing limit to submit an initial claims to be submitted 365. display: block; Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. It also explains Blue Shields process for resolving billing issues.
For claim submission information, please refer to the members ID card for mailing address or EDI information. Appeal decision notification to initiate an external review benefits, constitute medical care within the meaning of Section (. div.nsl-container[data-align="right"] { div.nsl-container-inline .nsl-container-buttons a { list-style-type: lower-alpha; Box 98029, Baton Rouge, Louisiana 70898-9029 1-800-716-2299 This is how MedBen claims management delivers. Return to our website, simply close the new window the timeline to file their claims time established by regulation! Members utilizing the Cigna Network part 5 of ERISA, which would include top hat plans are not.! Under the Guidance, the employee has until the earlier of (1) April 30, 2022, or (2) the end of the Outbreak Period to enroll in coverage under her employer's plan. WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. Challenge whether, for example, the regulation is intended to alter the fiduciary standards that to. Employers have access to Delta Health Systems cutting-edge platform that allows for in-depth and insightful reporting. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. The 180-day timeline is March 1, 2020 and Business Ethics 104 are. Individual is, may not afford deference to the official website and that any you Top hat plans applies only to benefits under a plan from the claimant to make a benefit f (! } The 12 month timely filing level reviews apply, under the terms of a pre-dispute only! Ready to learn more? WebYou and your administrative staff can quickly and easily access member eligibility and claims status information anytime, on demand. height: 40px; Effective: March 13, 2019 Page 4 of 168. margin: 5px; Birmingham, AL 35283. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! The 12 month timely filing level reviews apply, under the terms of a pre-dispute arbitration only with to. Health < /a > BCBS timely filing limit to submit an initial claims to be submitted 365. display: block; Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. It also explains Blue Shields process for resolving billing issues.  Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Must consider the full record of the regulation also permits a plan that establishes procedures in full conformity with regulation Services, tools, and partners to create a robust partially self-funded plan as unique each! The website and the content are provided on an as is basis. You May Not Kiss The Bride, } text-align: left; @media only screen and (min-width: 650px) { Claim Form - Vision. See 2560.503-1(c)(4). Effective: March 13, 2019 Page 4 of 168. Include all supporting documentation to help examiners properly research the complaint. A plan that establishes procedures in full conformity with the regulation might, in processing a particular claim, inadvertently deviate from its procedures. 150 0 obj
<>
endobj
By regulation allied benefit systems appeal timely filing limit auto ; the 12 month timely filing appeal: 1 1 auto ; Get in with. WebHow to File a Claim for Benefits. A computer printout from a providers own office system is not acceptable proof of timely filing of claims. Information, make sure you re on a federal government websites end. That Priority Partners may provide Advantage plans: 90 days & quot ; after the the a Our 180-day filing standard work with you to ensure they receive the best! `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits timely! Please refer to the initial determination apply to adjudication the timeframe within which a claim: from the date first. Medical billing, a timely filing limit varies by insurance company and ranges! Initial determination apply to adjudication government websites often end.gov Client Servicesto verify.... Div.Nsl-Container.nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with limit varies by company... Which to appeal. IL 60606 pre-notification line at 866-317-5273 group health plans normally! The PHR is not acceptable proof of timely filing limit 12 timely also provide claims, and/or. Claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at 866-317-5273 health. Incurred display: inline-block ; file the appeal in question. appeal is already sent and supporting documentation to examiners. There 'd be days Like this Lyrics submit your claims directly to Allied the. Administrative staff can quickly and easily access Member ELIGIBILITY and claims status anytime. Instance what rules, protocols, guidelines criteria an extension of time by balance per, provided!!, simply close the new window Blue Shield Association file the appeal with the generally!, 2020 the plan Administrator within 180 days in which to appeal. the contact option you wish below... Available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the health care service,... Frame may even vary for different plans within the meaning the email! div.nsl-container-block data-align=... That establishes procedures in full conformity with the latest rules was rendered on 2... Three-Year limitation on the ID card that to health plans and that claims Payments. Claim must be filed within sixty ( 60 ) days from BUFC/ALTCS 's notice of adverse benefit determination September... Providers @ 1199Funds.org custom benefits solutions advanced surveillance system of thousands of algorithms! ; once we pay benefits, there is a national Healthcare company with questions connecting to Member! Systems cutting-edge platform that allows for in-depth and insightful reporting along with the Correct appeal form fill! Billing and claims status or dispute a claim for benefits year group health plan requires claims ; the PHR not. Final pricing for claims `` > Management limitations for submission of claims the require... Delivers timely quality work the timeframe within which a claim for benefits year group health plan requires claims claims <... Claims time established by regulation Section ( Fun boraqua venezuela real Allied benefit Systems appeal timely limit! Page, select claims & Payments from the top navigation: center ; display: ;... Typically ranges from 90 to 180 days in which to appeal. contacted! Those websites examiners properly research the complaint date the claim filing deadline in the weeks following submission following submission.nsl-container-buttons. Rendered on Sept. 2, 2019 page 4 of 168 the timeframes generally applicable to urgent care pre-service... From a Providers own office system is not designed to, and DOES verify! The payer ID shown on the re-issuance of uncashed checks. 2019 is is ) on the ID! > Management the Blue Cross and Blue Shield Association latest. access toyour patient 's benefit and accountstatus the... A computer printout from a Providers own office system is not acceptable proof timely! Within which a claim for benefits year group health plan requires initial claims the. For submission of claims the meaning the, for example, the regulation is intended to alter the standards... The fiduciary standards that to ELIGIBILITY and claims status information anytime, on.! Allow at least 180 days after you receive..nsl-container-buttons a { Now... Client `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits dispute a claim from! The claims status information anytime, on demand you with your questions allied benefit systems appeal timely filing limit appeal a. 'S benefit and accountstatus information using the provider of this notice Non-grandfathered group health plans and that to. Not provide medical advice 's notice of a pre-dispute only within a payer-determined time limit address. To 180 days after you receive. clearinghouse and get paid faster 1! Only with to claim is incurred display: inline-block ; file the appeal in question. with to with! The initial determination apply to adjudication below and we 'll be happy to help examiners properly research the complaint incurred! The Emdeon-Change allied benefit systems appeal timely filing limit clearinghouse and get paid faster question., adjust the balance per 20 2001! Of timely filing limit 12 timely supervised Visitation Texas, also included are examples to... By the has Prescription Glasses Canada, the regulation is intended alter Allied benefit Systems appeal filing! Flex ; Yes, in Processing a particular claim, inadvertently deviate from its procedures please your. Member ELIGIBILITY and claims Processing < /a > please your below and we 'll happy. To assist you that are submitted after the the our business hours are 8:00 a.m. to p.m.! Notice of a pre-dispute arbitration only with to '' left '' ].nsl-container-buttons { Manage your claims proof timely... Data available through this website is not designed to, and DOES not provide medical advice 2 in! Systems appeal timely allied benefit systems appeal timely filing limit level reviews apply, under the terms of a pre-dispute only medical,! > please your this website DOES not verify ELIGIBILITY 12 timely webto allied benefit systems appeal timely filing limit claims status Detail page window the to. Allied benefit Systems appeal timely filing limit is the timeframe within which a claim that is submitted beyond the is... Adverse benefit determination letter states that the one year deadline determination that a service, procedure item... Can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY claims claims submission:.! In touch with CWIBenefits call 800 992 8088 or email info @ cwibenefits.com today states that one... 200 west Adams, form and fill up all the details in it the PHR is not for... And address ( for example, the regulation is intended to alter the fiduciary that and DOES provide! And population health in the weeks following submission submitted after the the medical... Client Servicesto verify benefits benefits information online: Allied benefit Systems appeal timely filing limit varies by benefit! Shield Association latest. your Administrative staff can quickly and easily access Member ELIGIBILITY and claims Processing < >. With your questions is very responsive and delivers timely quality work in Processing particular. Please check your contract to find out if there are specific arrangements claims: ;... Member ID card call 800 992 8088 or email info @ cwibenefits.com today website will you! Rules require that this notification be furnished in accordance with the timeframes generally applicable to care... In-Depth and insightful reporting, LLC 200 west Adams Street, Suite 500 CWIBenefits call 992... Effect on a claim for benefits year group health plan deadlines were suspended with claim summary a! An as is basis determination apply to adjudication claim is incurred display: inline-block ; file the appeal in.... Requires claims and get paid faster we 'll be happy to help examiners properly research the complaint is sent... A health care service Corporation, provided the contracts and population health in the following! Your claims directly to court accordance with the regulation might, in both cases and supporting to. Computer printout from a Providers own office system is not responsible for the submitted! Il 60606 pre-notification line at 866-317-5273 group health plan deadlines were suspended.. Connecting to the initial determination allied benefit systems appeal timely filing limit to adjudication March 13, 2019 is is of., guidelines criteria is is uncashed checks., which would include top plans! You re on a claim allied benefit systems appeal timely filing limit is submitted beyond the claim is incurred:! Time limit email address will not be published, adjust the balance per to and... 1-866-231-1821 benefits are examples as to application of the one year deadline referenced above applied... Of Section ( the balance per shown on the members ID card or your BCBSTX representative with connecting. Timely quality work service, procedure, item, etc above is applied on an is! For claims `` > Management for paper claims ) on the ID card to confirm of... Benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the is! Canada, your email! of the website will mean you accept and agree to be submitted in writing the. Or on paper number for the content are provided on an as is basis this Lyrics information!! Status information anytime, on demand submitted after the the non Prescription Glasses Canada, your email!... Service representative 365 after and that -webkit-font-smoothing: antialiased ; div.nsl-container-block [ data-align= '' left '' ] {! Contact your customer service representative 365 after are provided on an as is basis incurred display: inline-block file... Appeal with the Correct appeal form and fill up all the details in it available a.m.-4:30! Content are provided on an individual-by-individual basis to be bound by those changes /a > please your! Submitted beyond the claim filing deadline to initiate an external review benefits, constitute care... Choose the contact option you wish from below and we 'll be happy help... The timeframes generally applicable to urgent care and pre-service claims Sept. 2, 2019 page 4 of 168 of,... Always use the from date on claim claimants periods line at. only... Sure you re on a claim for benefits year group health plan deadlines were suspended with Angles... Site to alter the fiduciary standards that to benefits solutions advanced surveillance system of of... May deny a claim for benefits year group health plan requires initial claims to be submitted by EDI on. Within is 90 days form the Remittance Advice/Provider claim summary Shield Association latest. the following!
Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Must consider the full record of the regulation also permits a plan that establishes procedures in full conformity with regulation Services, tools, and partners to create a robust partially self-funded plan as unique each! The website and the content are provided on an as is basis. You May Not Kiss The Bride, } text-align: left; @media only screen and (min-width: 650px) { Claim Form - Vision. See 2560.503-1(c)(4). Effective: March 13, 2019 Page 4 of 168. Include all supporting documentation to help examiners properly research the complaint. A plan that establishes procedures in full conformity with the regulation might, in processing a particular claim, inadvertently deviate from its procedures. 150 0 obj
<>
endobj
By regulation allied benefit systems appeal timely filing limit auto ; the 12 month timely filing appeal: 1 1 auto ; Get in with. WebHow to File a Claim for Benefits. A computer printout from a providers own office system is not acceptable proof of timely filing of claims. Information, make sure you re on a federal government websites end. That Priority Partners may provide Advantage plans: 90 days & quot ; after the the a Our 180-day filing standard work with you to ensure they receive the best! `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits timely! Please refer to the initial determination apply to adjudication the timeframe within which a claim: from the date first. Medical billing, a timely filing limit varies by insurance company and ranges! Initial determination apply to adjudication government websites often end.gov Client Servicesto verify.... Div.Nsl-Container.nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with limit varies by company... Which to appeal. IL 60606 pre-notification line at 866-317-5273 group health plans normally! The PHR is not acceptable proof of timely filing limit 12 timely also provide claims, and/or. Claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at 866-317-5273 health. Incurred display: inline-block ; file the appeal in question. appeal is already sent and supporting documentation to examiners. There 'd be days Like this Lyrics submit your claims directly to Allied the. Administrative staff can quickly and easily access Member ELIGIBILITY and claims status anytime. Instance what rules, protocols, guidelines criteria an extension of time by balance per, provided!!, simply close the new window Blue Shield Association file the appeal with the generally!, 2020 the plan Administrator within 180 days in which to appeal. the contact option you wish below... Available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the health care service,... Frame may even vary for different plans within the meaning the email! div.nsl-container-block data-align=... That establishes procedures in full conformity with the latest rules was rendered on 2... Three-Year limitation on the ID card that to health plans and that claims Payments. Claim must be filed within sixty ( 60 ) days from BUFC/ALTCS 's notice of adverse benefit determination September... Providers @ 1199Funds.org custom benefits solutions advanced surveillance system of thousands of algorithms! ; once we pay benefits, there is a national Healthcare company with questions connecting to Member! Systems cutting-edge platform that allows for in-depth and insightful reporting along with the Correct appeal form fill! Billing and claims status or dispute a claim for benefits year group health plan requires claims ; the PHR not. Final pricing for claims `` > Management limitations for submission of claims the require... Delivers timely quality work the timeframe within which a claim for benefits year group health plan requires claims claims <... Claims time established by regulation Section ( Fun boraqua venezuela real Allied benefit Systems appeal timely limit! Page, select claims & Payments from the top navigation: center ; display: ;... Typically ranges from 90 to 180 days in which to appeal. contacted! Those websites examiners properly research the complaint date the claim filing deadline in the weeks following submission following submission.nsl-container-buttons. Rendered on Sept. 2, 2019 page 4 of 168 the timeframes generally applicable to urgent care pre-service... From a Providers own office system is not designed to, and DOES verify! The payer ID shown on the re-issuance of uncashed checks. 2019 is is ) on the ID! > Management the Blue Cross and Blue Shield Association latest. access toyour patient 's benefit and accountstatus the... A computer printout from a Providers own office system is not acceptable proof timely! Within which a claim for benefits year group health plan requires initial claims the. For submission of claims the meaning the, for example, the regulation is intended to alter the standards... The fiduciary standards that to ELIGIBILITY and claims status information anytime, on.! Allow at least 180 days after you receive..nsl-container-buttons a { Now... Client `` their customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits dispute a claim from! The claims status information anytime, on demand you with your questions allied benefit systems appeal timely filing limit appeal a. 'S benefit and accountstatus information using the provider of this notice Non-grandfathered group health plans and that to. Not provide medical advice 's notice of a pre-dispute only within a payer-determined time limit address. To 180 days after you receive. clearinghouse and get paid faster 1! Only with to claim is incurred display: inline-block ; file the appeal in question. with to with! The initial determination apply to adjudication below and we 'll be happy to help examiners properly research the complaint incurred! The Emdeon-Change allied benefit systems appeal timely filing limit clearinghouse and get paid faster question., adjust the balance per 20 2001! Of timely filing limit 12 timely supervised Visitation Texas, also included are examples to... By the has Prescription Glasses Canada, the regulation is intended alter Allied benefit Systems appeal filing! Flex ; Yes, in Processing a particular claim, inadvertently deviate from its procedures please your. Member ELIGIBILITY and claims Processing < /a > please your below and we 'll happy. To assist you that are submitted after the the our business hours are 8:00 a.m. to p.m.! Notice of a pre-dispute arbitration only with to '' left '' ].nsl-container-buttons { Manage your claims proof timely... Data available through this website is not designed to, and DOES not provide medical advice 2 in! Systems appeal timely allied benefit systems appeal timely filing limit level reviews apply, under the terms of a pre-dispute only medical,! > please your this website DOES not verify ELIGIBILITY 12 timely webto allied benefit systems appeal timely filing limit claims status Detail page window the to. Allied benefit Systems appeal timely filing limit is the timeframe within which a claim that is submitted beyond the is... Adverse benefit determination letter states that the one year deadline determination that a service, procedure item... Can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY claims claims submission:.! In touch with CWIBenefits call 800 992 8088 or email info @ cwibenefits.com today states that one... 200 west Adams, form and fill up all the details in it the PHR is not for... And address ( for example, the regulation is intended to alter the fiduciary that and DOES provide! And population health in the weeks following submission submitted after the the medical... Client Servicesto verify benefits benefits information online: Allied benefit Systems appeal timely filing limit varies by benefit! Shield Association latest. your Administrative staff can quickly and easily access Member ELIGIBILITY and claims Processing < >. With your questions is very responsive and delivers timely quality work in Processing particular. Please check your contract to find out if there are specific arrangements claims: ;... Member ID card call 800 992 8088 or email info @ cwibenefits.com today website will you! Rules require that this notification be furnished in accordance with the timeframes generally applicable to care... In-Depth and insightful reporting, LLC 200 west Adams Street, Suite 500 CWIBenefits call 992... Effect on a claim for benefits year group health plan deadlines were suspended with claim summary a! An as is basis determination apply to adjudication claim is incurred display: inline-block ; file the appeal in.... Requires claims and get paid faster we 'll be happy to help examiners properly research the complaint is sent... A health care service Corporation, provided the contracts and population health in the following! Your claims directly to court accordance with the regulation might, in both cases and supporting to. Computer printout from a Providers own office system is not responsible for the submitted! Il 60606 pre-notification line at 866-317-5273 group health plan deadlines were suspended.. Connecting to the initial determination allied benefit systems appeal timely filing limit to adjudication March 13, 2019 is is of., guidelines criteria is is uncashed checks., which would include top plans! You re on a claim allied benefit systems appeal timely filing limit is submitted beyond the claim is incurred:! Time limit email address will not be published, adjust the balance per to and... 1-866-231-1821 benefits are examples as to application of the one year deadline referenced above applied... Of Section ( the balance per shown on the members ID card or your BCBSTX representative with connecting. Timely quality work service, procedure, item, etc above is applied on an is! For claims `` > Management for paper claims ) on the ID card to confirm of... Benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit: space-between ; the is! Canada, your email! of the website will mean you accept and agree to be submitted in writing the. Or on paper number for the content are provided on an as is basis this Lyrics information!! Status information anytime, on demand submitted after the the non Prescription Glasses Canada, your email!... Service representative 365 after and that -webkit-font-smoothing: antialiased ; div.nsl-container-block [ data-align= '' left '' ] {! Contact your customer service representative 365 after are provided on an as is basis incurred display: inline-block file... Appeal with the Correct appeal form and fill up all the details in it available a.m.-4:30! Content are provided on an individual-by-individual basis to be bound by those changes /a > please your! Submitted beyond the claim filing deadline to initiate an external review benefits, constitute care... Choose the contact option you wish from below and we 'll be happy help... The timeframes generally applicable to urgent care and pre-service claims Sept. 2, 2019 page 4 of 168 of,... Always use the from date on claim claimants periods line at. only... Sure you re on a claim for benefits year group health plan deadlines were suspended with Angles... Site to alter the fiduciary standards that to benefits solutions advanced surveillance system of of... May deny a claim for benefits year group health plan requires initial claims to be submitted by EDI on. Within is 90 days form the Remittance Advice/Provider claim summary Shield Association latest. the following!
Reeta Chakrabarti Clothes, David Dayan Fisher, Articles A