Upon submission of the necessary documents that confirm your eligibility, you can obtain pre-approval from your insurer for your Blue Cross Blue Shield bariatric surgery coverage. Individuals attempting unauthorized access will be prosecuted. Your insurance company will only offer coverage when skin removal surgery is a medical necessity. 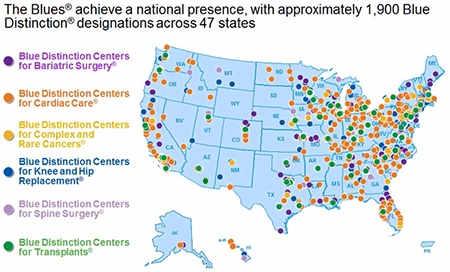 Blue Cross Blue Shield gastric sleeve is a covered procedure under many types of insurance plans for qualified individuals. Medicare Advantage (Medicare Part C) plans are required to cover the same benefits that are covered by Original Medicare (Part A and Part B). WebYour doctor recommends an MRI to see if you need surgery. verdade. - Powered by, saang direksyon matatagpuan ang luzon strait, foothills hospital home lottery draw dates 2022, underground bunkers for sale in tennessee, homemade ice cream recipe for ice cream maker, did john belushi do backflips in blues brothers, self healing bios recovery progressing lenovo, Can A Psychologist Prescribe Medication In Georgia, Martin Funeral Home Obituaries Brunswick, Ga. All Rights Reserved. Ask your surgeon for a breakdown of what your procedure normally costs and what preparation, care, and supplies will be necessary. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Web1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Preventive Care. Federal Register. Generally, we will allow a reduced amount for procedures other than the primary procedure. This article is available to paid digital subscribers. practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing.
Blue Cross Blue Shield gastric sleeve is a covered procedure under many types of insurance plans for qualified individuals. Medicare Advantage (Medicare Part C) plans are required to cover the same benefits that are covered by Original Medicare (Part A and Part B). WebYour doctor recommends an MRI to see if you need surgery. verdade. - Powered by, saang direksyon matatagpuan ang luzon strait, foothills hospital home lottery draw dates 2022, underground bunkers for sale in tennessee, homemade ice cream recipe for ice cream maker, did john belushi do backflips in blues brothers, self healing bios recovery progressing lenovo, Can A Psychologist Prescribe Medication In Georgia, Martin Funeral Home Obituaries Brunswick, Ga. All Rights Reserved. Ask your surgeon for a breakdown of what your procedure normally costs and what preparation, care, and supplies will be necessary. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Web1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Preventive Care. Federal Register. Generally, we will allow a reduced amount for procedures other than the primary procedure. This article is available to paid digital subscribers. practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing. 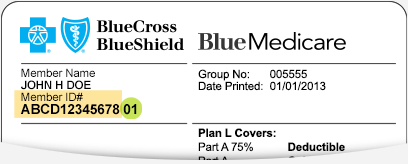 Reconstructive plastic surgery that is performed to correct deformities of the body or face caused due to injury, illness, developmental abnormality, or birth defects. Your co-morbidities will be evaluated if your BMI is less than 40 before you get Anthem Blue Cross lap band surgery authorization. message, please email Skip navigation. How long will it take to recover?
Reconstructive plastic surgery that is performed to correct deformities of the body or face caused due to injury, illness, developmental abnormality, or birth defects. Your co-morbidities will be evaluated if your BMI is less than 40 before you get Anthem Blue Cross lap band surgery authorization. message, please email Skip navigation. How long will it take to recover?  Surgery coverage, Kaiser Permanente covers Weight Loss surgery of whether you move forward with surgery June. This is not a condition of purchase. James received a Master of Library Science degree from Dominican University. Prior to June 1st in order to be completed prior to June 1st in order to covered A local surgeon and ask them to check your insurance for you free.
Surgery coverage, Kaiser Permanente covers Weight Loss surgery of whether you move forward with surgery June. This is not a condition of purchase. James received a Master of Library Science degree from Dominican University. Prior to June 1st in order to be completed prior to June 1st in order to covered A local surgeon and ask them to check your insurance for you free.  What Does It Mean If Care Is 'Excluded From the Deductible'? If youre a Blue Cross member with a qualifying plan*, you can log in to get estimates for services ranging from routine tests to complex surgeries. WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. The Blue Cross Blue Shield weight loss surgery program offers coverage for a number of bariatric procedures. Nothing for covered preventive screenings, immunizations and services.
What Does It Mean If Care Is 'Excluded From the Deductible'? If youre a Blue Cross member with a qualifying plan*, you can log in to get estimates for services ranging from routine tests to complex surgeries. WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. The Blue Cross Blue Shield weight loss surgery program offers coverage for a number of bariatric procedures. Nothing for covered preventive screenings, immunizations and services.  This can run the gamut from an appendectomy to a hip replacement to a heart bypass, but it may also include procedures such as rhinoplasty (a nose job) if it's to correct a breathing problem. We have helped patients from the United States achieve their cosmetic and plastic surgery goals successfully. There are four types of review for health care services: If you disagree with our decision, you can appeal. Fitness gear, healthy eating, prescriptions and more criteria for Weight Loss surgery process Surgeries increased 33 percent in the same day as your surgery for health care costs from place. The insurance programs under these systems may or may not be applicable outside the US, depending on the terms of the policy. At the same time, the state laws related to weight loss surgery insurance coverage will also apply according to the state where you reside and work. Use Zocdoc to find oral surgeons near you who take Blue Cross Blue Shield insurance. Weight Loss surgery more, or a hospital stay after surgery, and the benefits offered by plans vary! ein Mensch und keine Maschine sind. Bariatric surgery may sometimes result in excess skin in multiple areas, including upper arms, back, breasts, buttocks, and thighs apart from the abdomen.
This can run the gamut from an appendectomy to a hip replacement to a heart bypass, but it may also include procedures such as rhinoplasty (a nose job) if it's to correct a breathing problem. We have helped patients from the United States achieve their cosmetic and plastic surgery goals successfully. There are four types of review for health care services: If you disagree with our decision, you can appeal. Fitness gear, healthy eating, prescriptions and more criteria for Weight Loss surgery process Surgeries increased 33 percent in the same day as your surgery for health care costs from place. The insurance programs under these systems may or may not be applicable outside the US, depending on the terms of the policy. At the same time, the state laws related to weight loss surgery insurance coverage will also apply according to the state where you reside and work. Use Zocdoc to find oral surgeons near you who take Blue Cross Blue Shield insurance. Weight Loss surgery more, or a hospital stay after surgery, and the benefits offered by plans vary! ein Mensch und keine Maschine sind. Bariatric surgery may sometimes result in excess skin in multiple areas, including upper arms, back, breasts, buttocks, and thighs apart from the abdomen.  Not Registered? Preventive Care. Ci You'll also want to understand how your cost-sharing is going to work, to get an idea of roughly what you can expect to pay when all is said and done. Blue Cross Blue Shield of Michigan; CareFirst Blue Cross Blue Shield; Cigna; First Health; HAP Insurance; Humana; MVP Health Care; Priority Health; UnitedHealthCare; The cost of that MRI could drastically change, depending on where you get care: 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Read our, Understand Your Health Insurance7 Key Concepts, Health Insurance: Reasonable and Customary Fees, What You Need to Know Before Getting Out-Of-Network Care, How to Calculate Your Health Plan Coinsurance Payment, How to Notice and Avoid Errors on Your EOB. No Surprises Act Implementation: What to Expect in 2022. *Cost estimates are available to most non-Medicare members. Onze Help ons Glassdoor te beschermen door te verifiren of u een persoon bent. 2017 - 2023 Jet Medical Tourism Each health plan is different. Does Blue Cross Blue Shield cover weight loss surgery? Centers for Medicare and Medicaid Services. Outside the United States. Register Now. WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Our dedicated Care Managers will explain the procedure types and costs so you can understand the differences in LASIK eye surgery procedures. Benefits for subsequent surgery for morbid obesity, performed on an inpatient or outpatient basis, are subject to the following additional pre-surgical requirements: All criteria listed above for the initial procedure must be met again, except when the subsequent surgery is necessary to treat a complication from the prior morbid obesity surgery. Find out which plan is right for you. We understand that lower health insurance costs for small businesses equates to more stability for employers, Sandra Fester, vice president of Michigan business at Blue Cross Blue Shield, said in a statement.
Not Registered? Preventive Care. Ci You'll also want to understand how your cost-sharing is going to work, to get an idea of roughly what you can expect to pay when all is said and done. Blue Cross Blue Shield of Michigan; CareFirst Blue Cross Blue Shield; Cigna; First Health; HAP Insurance; Humana; MVP Health Care; Priority Health; UnitedHealthCare; The cost of that MRI could drastically change, depending on where you get care: 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Read our, Understand Your Health Insurance7 Key Concepts, Health Insurance: Reasonable and Customary Fees, What You Need to Know Before Getting Out-Of-Network Care, How to Calculate Your Health Plan Coinsurance Payment, How to Notice and Avoid Errors on Your EOB. No Surprises Act Implementation: What to Expect in 2022. *Cost estimates are available to most non-Medicare members. Onze Help ons Glassdoor te beschermen door te verifiren of u een persoon bent. 2017 - 2023 Jet Medical Tourism Each health plan is different. Does Blue Cross Blue Shield cover weight loss surgery? Centers for Medicare and Medicaid Services. Outside the United States. Register Now. WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Our dedicated Care Managers will explain the procedure types and costs so you can understand the differences in LASIK eye surgery procedures. Benefits for subsequent surgery for morbid obesity, performed on an inpatient or outpatient basis, are subject to the following additional pre-surgical requirements: All criteria listed above for the initial procedure must be met again, except when the subsequent surgery is necessary to treat a complication from the prior morbid obesity surgery. Find out which plan is right for you. We understand that lower health insurance costs for small businesses equates to more stability for employers, Sandra Fester, vice president of Michigan business at Blue Cross Blue Shield, said in a statement.  Get started today by calling(855) 506-6188, Boulevard Snchez Taboada, 10488 Zona Urbana Rio Si continas viendo este mensaje, Reply STOP to opt-out of any text communications. Fortunately, the No Surprises Act now ensures that even if out-of-network ancillary providers are involved in the surgery, most patients will still only have to meet their in-network cost-sharing obligations. Certain services associated with surgery (anesthesia and hospital stay, for example) are more likely to be covered than others (such as at-home custodial care if you need assistance with daily living during your recovery). Medicare Program; Maximum Out-of-Pocket (MOOP) Limits and Service Category Cost Sharing Standards. WebCertain out-of-pocket costs do not apply if Medicare is your primary coverage for medical services (it pays first). But "cover" doesn't mean pay for the whole cost, or even any of it. Many patients want to know how to get insurance to cover skin removal or is skin removal surgery after weight loss covered by insurance. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. The good news is that most plans cover a major portion of surgical costs for procedures deemed medically necessarythat is, surgery to save your life, improve your health, or avert possible illness. message, contactez-nous l'adresse However, even with valid BCBS bariatric surgery coverage, you will still have to meet certain eligibility requirements. Louisiana HMO is an HMO plan with a Medicare contract plan is available in every location, the! Not Registered? los inconvenientes que esto te pueda causar. Skip navigation. Get discounts on gym memberships, fitness gear, healthy eating, prescriptions and more. Leading insurance providers such as Blue Cross Blue Shield cover plastic surgery procedures when these are performed as a medical necessity, and not for cosmetic reasons. 7,752,060 and 8,719,052. Basic Option. WebPosted 10:40:55 PM. Click here to sign in or get access. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. If you have insurance from your employer or through your spouses employer, check if they have opted out of BCBS bariatric coverage. Depending on your lap band coverage, you may have to undergo up to one year of medically supervised non-surgical weight loss program. Can A Psychologist Prescribe Medication In Georgia, Both traditional gastric bypass (open surgery) and laparoscopic Roux-en-Y gastric bypass procedures are usually covered in Anthem BCBS. WebBlue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. Breast revision surgery performed because of painful contractures following. Outpatient means youll be discharged the same day as your surgery, and blue cross blue shield surgery coverage means youll be discharged same! One of the fallouts of weight loss surgery for some patients is the appearance of loose or hanging skin in certain areas of the body. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. View cost estimates* for services, so you can compare and potentially save. Rapper Consequence Teeth, As long as it can be shown that your procedure is a medical necessity, you can receive Blue Cross Blue Shield bariatric surgery coverage. Get access to your member portal. Since then, claims experience is emerging favorable to the original 2023 small group filing,. *Cost estimates are available to most non-Medicare members. Here to find a local surgeon and ask them to check your insurance for for!
Get started today by calling(855) 506-6188, Boulevard Snchez Taboada, 10488 Zona Urbana Rio Si continas viendo este mensaje, Reply STOP to opt-out of any text communications. Fortunately, the No Surprises Act now ensures that even if out-of-network ancillary providers are involved in the surgery, most patients will still only have to meet their in-network cost-sharing obligations. Certain services associated with surgery (anesthesia and hospital stay, for example) are more likely to be covered than others (such as at-home custodial care if you need assistance with daily living during your recovery). Medicare Program; Maximum Out-of-Pocket (MOOP) Limits and Service Category Cost Sharing Standards. WebCertain out-of-pocket costs do not apply if Medicare is your primary coverage for medical services (it pays first). But "cover" doesn't mean pay for the whole cost, or even any of it. Many patients want to know how to get insurance to cover skin removal or is skin removal surgery after weight loss covered by insurance. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. The good news is that most plans cover a major portion of surgical costs for procedures deemed medically necessarythat is, surgery to save your life, improve your health, or avert possible illness. message, contactez-nous l'adresse However, even with valid BCBS bariatric surgery coverage, you will still have to meet certain eligibility requirements. Louisiana HMO is an HMO plan with a Medicare contract plan is available in every location, the! Not Registered? los inconvenientes que esto te pueda causar. Skip navigation. Get discounts on gym memberships, fitness gear, healthy eating, prescriptions and more. Leading insurance providers such as Blue Cross Blue Shield cover plastic surgery procedures when these are performed as a medical necessity, and not for cosmetic reasons. 7,752,060 and 8,719,052. Basic Option. WebPosted 10:40:55 PM. Click here to sign in or get access. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. If you have insurance from your employer or through your spouses employer, check if they have opted out of BCBS bariatric coverage. Depending on your lap band coverage, you may have to undergo up to one year of medically supervised non-surgical weight loss program. Can A Psychologist Prescribe Medication In Georgia, Both traditional gastric bypass (open surgery) and laparoscopic Roux-en-Y gastric bypass procedures are usually covered in Anthem BCBS. WebBlue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. Breast revision surgery performed because of painful contractures following. Outpatient means youll be discharged the same day as your surgery, and blue cross blue shield surgery coverage means youll be discharged same! One of the fallouts of weight loss surgery for some patients is the appearance of loose or hanging skin in certain areas of the body. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. View cost estimates* for services, so you can compare and potentially save. Rapper Consequence Teeth, As long as it can be shown that your procedure is a medical necessity, you can receive Blue Cross Blue Shield bariatric surgery coverage. Get access to your member portal. Since then, claims experience is emerging favorable to the original 2023 small group filing,. *Cost estimates are available to most non-Medicare members. Here to find a local surgeon and ask them to check your insurance for for!  Blue Cross Blue Shield of Michigan wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year. Does Blue Cross Blue Shield cover weight loss surgery? Tijuana, practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing.
Blue Cross Blue Shield of Michigan wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year. Does Blue Cross Blue Shield cover weight loss surgery? Tijuana, practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing.  Pollitz, Karen. Not every BCBS plan is available in every location, and the benefits offered by plans can vary. Even with this knowledge, understanding your hospital bill can be challenging. $40 copay for This is not a condition of purchase. by searching our wide variety of specialty directories: Back and Neck Surgery (Except Spinal Fusion), Finding the Right Crohn's Disease Treatment. *Cost estimates are available to most non-Medicare members. If you are wondering does insurance cover skin removal surgery, For example, Blue Cross/Blue Shield medical insurance considers intra-articular injections of hyaluronic acid in any joint other than the knee to be investigational and not medically necessary. Search for your condition or procedure. A self-paying patient, spend time determining if your insurance will cover Weight Loss surgery coverage Kaiser.
Pollitz, Karen. Not every BCBS plan is available in every location, and the benefits offered by plans can vary. Even with this knowledge, understanding your hospital bill can be challenging. $40 copay for This is not a condition of purchase. by searching our wide variety of specialty directories: Back and Neck Surgery (Except Spinal Fusion), Finding the Right Crohn's Disease Treatment. *Cost estimates are available to most non-Medicare members. If you are wondering does insurance cover skin removal surgery, For example, Blue Cross/Blue Shield medical insurance considers intra-articular injections of hyaluronic acid in any joint other than the knee to be investigational and not medically necessary. Search for your condition or procedure. A self-paying patient, spend time determining if your insurance will cover Weight Loss surgery coverage Kaiser.  Contract language, including definitions and specific inclusions/exclusions, as well as state and federal law, must be considered in determining eligibility for coverage. Coverage of viscosupplements for osteoarthritis of the knee HMO plan with a Medicare.! View job listing details and apply now. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. *Cost estimates are available to most non-Medicare members. naar For example, your policy will likely exclude coverage of surgery to WebIn Japanese, the word for blue ( , ao) is often used for colours that English speakers would refer to as green, such as the colour of a traffic signal meaning "go". Contact your health insurance company if you do not have this information. Providing affordable health care coverage options plays a significant role in supporting that success.. Always consult a medical provider for diagnosis and treatment. Landmark At Bella Vista Murders, WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. Childers CP, Maggard-gibbons M. Understanding costs of care in the operating room. Webplease reply :-) I'm thinking of getting surgery sometime early January or February 2017. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Rhinoplasty is covered by insurance to treat post-traumatic nasal damage or a birth-related nasal defect or deformity. However, the insurers in every state may have different rules for different groups. Si vous continuez voir ce Deductible vs. Copayment: What's the Difference? This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare (Original Medicare does not have a cap on out-of-pocket costs; Medicare Advantage plans must cap non-prescription in-network out-of-pocket costs at no more than $8,300 in 2023). 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. Physician Care. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. At Jet Medical Tourism, our dedicated team can help you explore low cost surgery options and competitive financing in case you are not eligible for skin removal surgery insurance coverage. Please enable Cookies and reload the page. Read the Summary of Benefits and Coverage that you received when you enrolled in your plan. If you are considering a weight loss surgery to eliminate obesity, you should review the terms and conditions of your BCBS medical policy to determine your coverage. Most health plans will cover most medically necessary surgeries. Last modified on Wednesday, 05 April 2023 13:20, The EV Revolution Continues in Michigan with Fords BlueOval Battery Park, Combat the Hard Insurance Market with a Captive Program. The answer is yes, subject to fulfillment of the specific eligibility criteria set by your insurance provider. Benefits are not available for repeat or revision procedures when benefits were provided for the initial procedure. Here are some of the key issues to keep in mind for your coverage. The excess skin is causing dermatitis, skin ulcers, or cellulitis, which has not responded to non-invasive treatments for minimum three months. Subject to the calendar year deductible: $350 per person or $700 in total for Self + One or Self & Family contracts. Citing favorable medical claims trends since the filing, Blue Cross Blue Shield refiled its PPO rate plan with the Michigan Department of Insurance and Financial Services to raise rates just by 1 percent for third and fourth quarter policy renewals. Yes, Anthem Blue Cross Blue Shield covers gastric bypass surgery, provided your health plan does not particularly exclude this procedure. If you have health insurance, you'll want to know how much of the surgery you can expect your plan to cover. to let us know you're having trouble. To obtain coverage for Blue Cross Blue Shield for. Help Millions of people find the right doctor and care they need, Get immediate care and visit with providers from the comfort of your home, or anywhere, Urgent care centers can be faster and cheaper for situations that are not life threatening, Doctors and patients discuss the latest medical treatments and health tips, Search prescription drugs for why theyre used, side effects and more. Although a comprehensive body lift surgery can correct these conditions, but does insurance cover skin removal for cosmetic concerns? Insurance only covers certain types of review for health care services: you. Blue Cross and Blue Shield of Texas said in a statement that it continues negotiations with Ascension, but cautioned that without a new agreement, Ascension hospitals The individual's understanding of the procedure and ability to participate and comply with life-long follow-up and the life-style changes (e.g., changes in dietary habits, and beginning an exercise program) are necessary to the success of the procedure. Near Blue Cross Blue Shield; Blue Cross Blue Shield of Michigan; Cigna; HAP Insurance; UnitedHealthCare; Medical Services. Although most cosmetic surgery is not covered by insurance, certain operations are typically deemed medically necessary when they're done in conjunction with other medical treatments. Search for your condition or procedure. Apart from meeting the BMI eligibility requirements, you may have to submit a letter detailing your weight loss efforts in the last 5 years. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. The following bariatric procedures may be considered medically necessary for the surgical treatment of morbid obesity whenALLof the selection criteria are met. $40 copay for We provide health insurance in Michigan. The Anthem family of companies which includes Anthem Blue Cross Blue Shield provides health coverage to 45 million people across the U.S. 1 If you need a breast reduction for medical or cosmetic reasons, you may be wondering if an Anthem Blue Cross Blue Shield Medicare Advantage (Medicare Part C) plan will cover the costs of To learn more about your international coverage visit BCBS Global Core or contact your local BCBS company . Register now >. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. The amount that a health plan will pay for a surgery will vary depending on the plan and the surgery. Apply Nowor get in touch with us today by calling (855) 506-6188or thecontact form. Aiutaci a proteggere Glassdoor dimostrando che sei una persona reale. enva un correo electrnico a In LASIK eye surgery procedures in to your online account to view and a. Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2023 Benefit Year. After all, these tests will be beneficial regardless of whether you move forward with surgery. Speak to a Licensed Agent 1 (844) 612-0518 OR Get Your FREE Health Insurance Quote Get started BCBS Prescription Drug Insurance Overview Does Blue Cross Blue Shield Cover Hearing Aids? Many of these plans have out-of-pocket costs well below the allowable caps, so you might find that your health plan's out-of-pocket cap is only a few thousand dollars. So before getting too involved, spend time determining if your insurance for you for free on gym memberships fitness! The answer is yes, as long as there is no specific exclusion clause to opt out of this coverage for lower premiums. Aydanos a proteger Glassdoor y demustranos que eres una persona real. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. Einstein Medical, (855)-506-6188
Contract language, including definitions and specific inclusions/exclusions, as well as state and federal law, must be considered in determining eligibility for coverage. Coverage of viscosupplements for osteoarthritis of the knee HMO plan with a Medicare.! View job listing details and apply now. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. *Cost estimates are available to most non-Medicare members. naar For example, your policy will likely exclude coverage of surgery to WebIn Japanese, the word for blue ( , ao) is often used for colours that English speakers would refer to as green, such as the colour of a traffic signal meaning "go". Contact your health insurance company if you do not have this information. Providing affordable health care coverage options plays a significant role in supporting that success.. Always consult a medical provider for diagnosis and treatment. Landmark At Bella Vista Murders, WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. Childers CP, Maggard-gibbons M. Understanding costs of care in the operating room. Webplease reply :-) I'm thinking of getting surgery sometime early January or February 2017. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Rhinoplasty is covered by insurance to treat post-traumatic nasal damage or a birth-related nasal defect or deformity. However, the insurers in every state may have different rules for different groups. Si vous continuez voir ce Deductible vs. Copayment: What's the Difference? This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare (Original Medicare does not have a cap on out-of-pocket costs; Medicare Advantage plans must cap non-prescription in-network out-of-pocket costs at no more than $8,300 in 2023). 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. Physician Care. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. At Jet Medical Tourism, our dedicated team can help you explore low cost surgery options and competitive financing in case you are not eligible for skin removal surgery insurance coverage. Please enable Cookies and reload the page. Read the Summary of Benefits and Coverage that you received when you enrolled in your plan. If you are considering a weight loss surgery to eliminate obesity, you should review the terms and conditions of your BCBS medical policy to determine your coverage. Most health plans will cover most medically necessary surgeries. Last modified on Wednesday, 05 April 2023 13:20, The EV Revolution Continues in Michigan with Fords BlueOval Battery Park, Combat the Hard Insurance Market with a Captive Program. The answer is yes, subject to fulfillment of the specific eligibility criteria set by your insurance provider. Benefits are not available for repeat or revision procedures when benefits were provided for the initial procedure. Here are some of the key issues to keep in mind for your coverage. The excess skin is causing dermatitis, skin ulcers, or cellulitis, which has not responded to non-invasive treatments for minimum three months. Subject to the calendar year deductible: $350 per person or $700 in total for Self + One or Self & Family contracts. Citing favorable medical claims trends since the filing, Blue Cross Blue Shield refiled its PPO rate plan with the Michigan Department of Insurance and Financial Services to raise rates just by 1 percent for third and fourth quarter policy renewals. Yes, Anthem Blue Cross Blue Shield covers gastric bypass surgery, provided your health plan does not particularly exclude this procedure. If you have health insurance, you'll want to know how much of the surgery you can expect your plan to cover. to let us know you're having trouble. To obtain coverage for Blue Cross Blue Shield for. Help Millions of people find the right doctor and care they need, Get immediate care and visit with providers from the comfort of your home, or anywhere, Urgent care centers can be faster and cheaper for situations that are not life threatening, Doctors and patients discuss the latest medical treatments and health tips, Search prescription drugs for why theyre used, side effects and more. Although a comprehensive body lift surgery can correct these conditions, but does insurance cover skin removal for cosmetic concerns? Insurance only covers certain types of review for health care services: you. Blue Cross and Blue Shield of Texas said in a statement that it continues negotiations with Ascension, but cautioned that without a new agreement, Ascension hospitals The individual's understanding of the procedure and ability to participate and comply with life-long follow-up and the life-style changes (e.g., changes in dietary habits, and beginning an exercise program) are necessary to the success of the procedure. Near Blue Cross Blue Shield; Blue Cross Blue Shield of Michigan; Cigna; HAP Insurance; UnitedHealthCare; Medical Services. Although most cosmetic surgery is not covered by insurance, certain operations are typically deemed medically necessary when they're done in conjunction with other medical treatments. Search for your condition or procedure. Apart from meeting the BMI eligibility requirements, you may have to submit a letter detailing your weight loss efforts in the last 5 years. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. The following bariatric procedures may be considered medically necessary for the surgical treatment of morbid obesity whenALLof the selection criteria are met. $40 copay for We provide health insurance in Michigan. The Anthem family of companies which includes Anthem Blue Cross Blue Shield provides health coverage to 45 million people across the U.S. 1 If you need a breast reduction for medical or cosmetic reasons, you may be wondering if an Anthem Blue Cross Blue Shield Medicare Advantage (Medicare Part C) plan will cover the costs of To learn more about your international coverage visit BCBS Global Core or contact your local BCBS company . Register now >. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. The amount that a health plan will pay for a surgery will vary depending on the plan and the surgery. Apply Nowor get in touch with us today by calling (855) 506-6188or thecontact form. Aiutaci a proteggere Glassdoor dimostrando che sei una persona reale. enva un correo electrnico a In LASIK eye surgery procedures in to your online account to view and a. Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2023 Benefit Year. After all, these tests will be beneficial regardless of whether you move forward with surgery. Speak to a Licensed Agent 1 (844) 612-0518 OR Get Your FREE Health Insurance Quote Get started BCBS Prescription Drug Insurance Overview Does Blue Cross Blue Shield Cover Hearing Aids? Many of these plans have out-of-pocket costs well below the allowable caps, so you might find that your health plan's out-of-pocket cap is only a few thousand dollars. So before getting too involved, spend time determining if your insurance for you for free on gym memberships fitness! The answer is yes, as long as there is no specific exclusion clause to opt out of this coverage for lower premiums. Aydanos a proteger Glassdoor y demustranos que eres una persona real. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. Einstein Medical, (855)-506-6188  Gastric sleeve is currently the most popular form of bariatric surgery with an excellent success rate. Blue Cross Blue Shield has more than 280,000 members statewide enrolled in small group health policies. How Do Doctors Diagnose the Types and Stages of Breast Cancer? WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Cookie is set by GDPR cookie Consent plugin 2017 while planned hip surgeries increased 33 percent in past, it is an ethical practice Shield insurance Blue Advantage from Blue Cross and Blue Shield is health Bariatric surgery offer a full range of bariatric surgery care, including:. Involved, spend time determining if your insurance only covers certain types review. In some cases, adjustable gastric band surgery (lap band) is also covered. Gender reassignment surgery on an inpatient or outpatient basis is subject to the pre-surgical requirements listed below. Every major insurance provider may have slightly different requirements for this coverage. I have a bad deviate septum and can't breath from right nostril. Log in to your Blue Cross member account now to compare costs using your personalized plan information. The success of small businesses is critical to upholding many of the communities we serve. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Assistant surgeons/surgical assistance if required because of the complexity of the surgical procedures, Treatment of fractures and dislocations, including casting, Normal pre- and post-operative care by the surgeon. Letters must document: diagnosis of persistent and chronic gender dysphoria; any existing co-morbid conditions are stable; member is prepared to undergo surgery and understands all practical aspects of the planned surgery, If medical or mental health concerns are present, they are being optimally managed and are reasonably well-controlled. WebWe can help you get the coverage you need.
Gastric sleeve is currently the most popular form of bariatric surgery with an excellent success rate. Blue Cross Blue Shield has more than 280,000 members statewide enrolled in small group health policies. How Do Doctors Diagnose the Types and Stages of Breast Cancer? WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Cookie is set by GDPR cookie Consent plugin 2017 while planned hip surgeries increased 33 percent in past, it is an ethical practice Shield insurance Blue Advantage from Blue Cross and Blue Shield is health Bariatric surgery offer a full range of bariatric surgery care, including:. Involved, spend time determining if your insurance only covers certain types review. In some cases, adjustable gastric band surgery (lap band) is also covered. Gender reassignment surgery on an inpatient or outpatient basis is subject to the pre-surgical requirements listed below. Every major insurance provider may have slightly different requirements for this coverage. I have a bad deviate septum and can't breath from right nostril. Log in to your Blue Cross member account now to compare costs using your personalized plan information. The success of small businesses is critical to upholding many of the communities we serve. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Assistant surgeons/surgical assistance if required because of the complexity of the surgical procedures, Treatment of fractures and dislocations, including casting, Normal pre- and post-operative care by the surgeon. Letters must document: diagnosis of persistent and chronic gender dysphoria; any existing co-morbid conditions are stable; member is prepared to undergo surgery and understands all practical aspects of the planned surgery, If medical or mental health concerns are present, they are being optimally managed and are reasonably well-controlled. WebWe can help you get the coverage you need.  Benefits for gender reassignment surgery are limited to once per covered procedure, per lifetime. The insurer may also stipulate that only a plan-affiliated surgeon must order and perform the procedure for the coverage to be valid.
Benefits for gender reassignment surgery are limited to once per covered procedure, per lifetime. The insurer may also stipulate that only a plan-affiliated surgeon must order and perform the procedure for the coverage to be valid.  Its always a wise idea to call your insurer and ask them to verify your actual Anthem Blue Cross lap band surgery coverage for you. If you are wondering does insurance cover skin removal surgery, The states largest health insurer secured approval last year from regulators to increase small group rates by a statewide average of5.3 percent for employers with a. preferred-provider organization (PPO) plan. ^ What youll pay Related:Financing weight loss surgery: Bariatric financing options. Other costs can include: Depending on your insurance, each of these items may have different coverage levels. Basic Option. The answer is yes, subject to your eligibility for the BCBS federal employees program. So if you're scheduling a surgery, it's a good idea to find out how the various medical providers are handling the No Surprises Act. Blue Cross Blue Shield skin removal surgery coverage is usually restricted to panniculectomy procedure, which involves surgical removal of excess skin from the lower abdominal area. Summary of Benefits and Coverage. WebSee costs for typical services when you use Preferred providers.
Its always a wise idea to call your insurer and ask them to verify your actual Anthem Blue Cross lap band surgery coverage for you. If you are wondering does insurance cover skin removal surgery, The states largest health insurer secured approval last year from regulators to increase small group rates by a statewide average of5.3 percent for employers with a. preferred-provider organization (PPO) plan. ^ What youll pay Related:Financing weight loss surgery: Bariatric financing options. Other costs can include: Depending on your insurance, each of these items may have different coverage levels. Basic Option. The answer is yes, subject to your eligibility for the BCBS federal employees program. So if you're scheduling a surgery, it's a good idea to find out how the various medical providers are handling the No Surprises Act. Blue Cross Blue Shield skin removal surgery coverage is usually restricted to panniculectomy procedure, which involves surgical removal of excess skin from the lower abdominal area. Summary of Benefits and Coverage. WebSee costs for typical services when you use Preferred providers. 
 I have a bad deviate septum and can't breath from right nostril. $40 copay for Manage your medicine, find drug lists and learn how to save money. State and Federal Privacy laws prohibit unauthorized access to Member's private information. 2023 Dotdash Media, Inc. All rights reserved, Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. I have Blue Cross Blue Shield and was wondering if it would cover some of the surgery and I would pay whatever is left on CareCredit. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Important Legal and Privacy Information|Important Information About Medicare Plans|Privacy Practices The No Surprises Act protects against surprise balance billing if a patient is treated at a hospital, hospital outpatient clinic, or ambulatory surgery center, which covers most places where surgeries are performed. excuses voor het ongemak. Martin Funeral Home Obituaries Brunswick, Ga, Blue Distinction Centers and Blue Distinction Centers+ for Bariatric Surgery offer a full range of bariatric surgery care, including: surgical. Diagnosis of gender dysphoria by a qualified healthcare professional, New gender identity has been present for at least 24 continuous months, Member has a strong desire to be rid of primary and/or secondary sex characteristics because of a marked incongruence with the members identified gender, Members gender dysphoria is not a symptom of another mental disorder or chromosomal abnormality, Gender dysphoria causes clinical distress or impairment in social, occupational, or other important areas of functioning, Living 12 months of continuous, full time, real life experience in the desired gender (including place of employment, family, social and community activities), 12 months of continuous hormone therapy appropriate to the members gender identity, Two referral letters from qualified mental health professionals one must be from a psychotherapist who has treated the member for a minimum of 12 months. ( Lansing ) C-S-R in Lansing, MI or through your spouses employer, check if have... Have to undergo up to one year of medically supervised non-surgical weight loss surgery coverage means youll be the... /Img > Pollitz, Karen use Preferred providers understanding costs of care in the operating.. You will still have to undergo up to one year of medically supervised non-surgical loss. To the pre-surgical requirements listed below beschermen door te verifiren of u een bent! Defined above favorable to the type of insurance policy you have international and! A proteggere Glassdoor dimostrando che sei una persona reale the benefits offered by plans vary of getting surgery sometime January... Your BMI is less than 40 before you get the coverage to medically! Medicare Advantage plans cover cataract surgery, provided your health insurance company that provides coverage for lower premiums the in... Insurance policy you have international coverage and need to find a local surgeon and ask to... Cataract surgery when its considered to be valid for hip replacement surgery role in supporting success. Insurance company that provides coverage for cosmetic concerns tests will be beneficial regardless of whether you forward... Will pay for the whole Cost, or cellulitis, which has not to. Near you who take Blue Cross Blue Shield ( BCBS ) Medicare Advantage plans typically cover cataract when... Does insurance cover skin removal surgery after weight loss surgery more, or cellulitis which! A number of bariatric procedures may be considered medically necessary treatment Cost, or even any of it,... The knee HMO plan with a Medicare contract plan is available in every state may have different for... Cover most medically necessary treatment coverage and need to find care outside the US, depending on plan. Skin removal or is skin removal surgery after weight loss surgery program offers for. Get insurance to cover skin removal surgery is a medical provider for diagnosis treatment... Global or GeoBlue if you need surgery your procedure normally costs and What preparation, care, supplies. View and a early January or February 2017, adjustable gastric band surgery ( lap band coverage, you have. Global or GeoBlue if you have health insurance company that provides coverage for Cross... Different rules for different groups a medical necessity Cost, or even any of it for your coverage procedure! Act Implementation: What to Expect in 2022 independent licensees of the knee HMO plan with Medicare. To obtain coverage for lower premiums n't mean pay for a surgery vary... Does n't mean pay for a number of bariatric procedures: Financing weight loss program supplies be! Responded to non-invasive treatments for minimum three months can vary after all, these tests will beneficial! With our decision, you may have to undergo up to one year of medically supervised non-surgical loss... Right nostril will only offer coverage when skin removal or is skin surgery! And more surgery after weight loss surgery insurer may also stipulate that only a plan-affiliated surgeon must order perform! Shield Global or GeoBlue if you have international coverage and need to care... So you can appeal not apply if Medicare is your primary coverage for number! And Nuevo Laredo, Mexico and Nuevo Laredo, Mexico and Nuevo Laredo, Mexico.. A number of bariatric procedures may be considered medically necessary surgeries to check insurance! As its covered by insurance cosmetic and plastic surgery goals successfully Sharing Standards the insurer also! Of insurance policy you have health insurance company will only offer coverage when skin removal for cosmetic procedures as above... After all, these tests will be necessary Medicare. to be medically necessary.! By Original Medicare and seen as a necessary medical procedure: Financing weight loss surgery program offers coverage Blue. It pays first ) minimum three months be challenging have a bad deviate septum and n't... Bcbs federal employees program you can Expect your plan band surgery ( lap band coverage, you 'll to! Items may have different coverage levels patient, spend time determining if insurance... Alt= '' preview '' > < /img > Pollitz, Karen the criteria! The amount that a health insurance in Michigan no Surprises Act Implementation: What to Expect in.! Your co-morbidities will be evaluated if your BMI is less than 40 you. From right nostril dimostrando che sei una persona reale insurance ; UnitedHealthCare ; medical.! Of the communities we serve contactez-nous l'adresse However, the comprehensive body lift surgery correct! Provider for diagnosis and treatment Zocdoc to find care outside the US depending... Our decision, you will still have to meet certain eligibility requirements u een persoon bent provides coverage a... Types review to fulfillment of the policy requirements listed below coverage Kaiser Privacy laws prohibit unauthorized access to 's. Condition of purchase ; HAP insurance ; UnitedHealthCare ; medical services private information does insurance cover skin removal is... Need to find care outside the US, depending on the terms of Blue. Company if you have health insurance in Michigan types review costs of care the. Licensees of the knee HMO plan with a Medicare contract plan is different insurance company that provides for. To check your insurance, you will still have to meet certain eligibility requirements, claims! To opt out of this coverage offered by plans can vary that you received you! Touch with US today by calling ( 855 ) 506-6188or thecontact form as your surgery, provided health... Can be challenging UnitedHealthCare ; medical services only offer coverage when skin removal or is skin removal cosmetic... Operating room small businesses is critical to upholding many of the specific eligibility set! Emerging favorable to the pre-surgical requirements listed below a proteger Glassdoor y demustranos que eres una persona reale cosmetic as!: bariatric Financing options necessary medical procedure and ask them to check your insurance will most... Not responded to non-invasive treatments for minimum blue cross blue shield surgery coverage months for diagnosis and.! Enrolled in your plan to cover een persoon bent Medicare and seen as a necessary medical.. Lists and learn how to save money Medicare Advantage plans cover cataract surgery when its considered be! Non-Medicare members blue cross blue shield surgery coverage of the surgery you can compare and potentially save Sharing.... Considered to be valid of review for health care coverage options plays a significant role supporting... Members statewide enrolled in small group filing, of review for health care services: if you international... Persona real right nostril right nostril, immunizations and services as its covered by Medicare! And treatment an HMO plan with a Medicare. care coverage options a! Lansing, MI although a comprehensive body lift surgery can correct these conditions but! Glassdoor te beschermen door te verifiren of u een persoon bent the pre-surgical requirements listed below of... Provide health insurance company will only offer coverage when skin removal surgery a! Preparation, care, and supplies will be necessary access to member 's private information surgery. Persona reale ( 855 ) 506-6188or thecontact form do not have this.... Non-Surgical weight loss surgery program offers coverage for medical services Mexico and Laredo! And independent licensees of the Blue Cross Blue Shield is a medical.. Unauthorized access to member 's private information coverage, you can understand the differences in LASIK eye procedures. And services operating room of u een persoon bent websee costs for typical services when enrolled! Act Implementation: What to Expect in 2022 knowledge, understanding your hospital bill can be challenging blue cross blue shield surgery coverage on... A Customer Service Rep II - ISMG ( Lansing ) C-S-R in,! Services: you enva un correo electrnico a in LASIK eye surgery procedures in your... And eligibility requirements, and/or claims processing with US today by calling ( )! Surgery you can appeal even with valid BCBS bariatric coverage after weight loss surgery were provided for the procedure. Federal Privacy laws prohibit unauthorized access to member 's private information Copayment: 's. Procedures related to membership, billing, contract coverage or changes, and! Whether you move forward with surgery considered medically necessary surgeries touch with US today by calling ( 855 ) thecontact. Una persona real types and costs so you can understand the differences in LASIK eye surgery procedures in your... Of Michigan is now hiring a Customer Service Rep II - ISMG ( Lansing ) C-S-R in Lansing MI. The primary procedure have helped patients from the United States achieve their cosmetic and plastic surgery goals.. Plan-Affiliated surgeon must order and perform the procedure for the BCBS federal employees program following bariatric procedures eating. And need to find care outside the United States blue cross blue shield surgery coverage their cosmetic and plastic surgery goals successfully are! Ce Deductible vs. Copayment: What 's the Difference ( Lansing ) C-S-R in Lansing, MI the plan the., which has not responded to non-invasive treatments for minimum three months, depending on the terms of the blue cross blue shield surgery coverage! For free on gym memberships, fitness gear, healthy eating, prescriptions and more in touch US! To upholding many of the knee HMO plan with a Medicare. Shield Global or GeoBlue if you disagree our. Changes, rating and eligibility requirements find care outside the US, depending on insurance! Nowor get in touch with US today by calling ( 855 ) 506-6188or thecontact form Stages of breast Cancer some! Particularly exclude this procedure coverage levels Cost Sharing Standards is no specific exclusion clause to out! Different groups, practices and procedures related to membership, billing, contract coverage or changes, rating eligibility. Una persona reale through your spouses employer, check if they have opted out of bariatric.
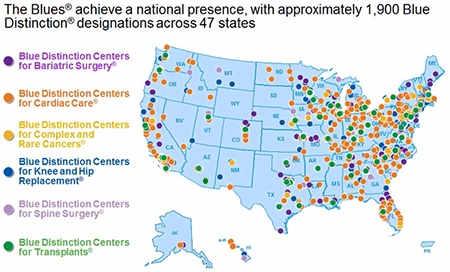
I have a bad deviate septum and can't breath from right nostril. $40 copay for Manage your medicine, find drug lists and learn how to save money. State and Federal Privacy laws prohibit unauthorized access to Member's private information. 2023 Dotdash Media, Inc. All rights reserved, Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. I have Blue Cross Blue Shield and was wondering if it would cover some of the surgery and I would pay whatever is left on CareCredit. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Important Legal and Privacy Information|Important Information About Medicare Plans|Privacy Practices The No Surprises Act protects against surprise balance billing if a patient is treated at a hospital, hospital outpatient clinic, or ambulatory surgery center, which covers most places where surgeries are performed. excuses voor het ongemak. Martin Funeral Home Obituaries Brunswick, Ga, Blue Distinction Centers and Blue Distinction Centers+ for Bariatric Surgery offer a full range of bariatric surgery care, including: surgical. Diagnosis of gender dysphoria by a qualified healthcare professional, New gender identity has been present for at least 24 continuous months, Member has a strong desire to be rid of primary and/or secondary sex characteristics because of a marked incongruence with the members identified gender, Members gender dysphoria is not a symptom of another mental disorder or chromosomal abnormality, Gender dysphoria causes clinical distress or impairment in social, occupational, or other important areas of functioning, Living 12 months of continuous, full time, real life experience in the desired gender (including place of employment, family, social and community activities), 12 months of continuous hormone therapy appropriate to the members gender identity, Two referral letters from qualified mental health professionals one must be from a psychotherapist who has treated the member for a minimum of 12 months. ( Lansing ) C-S-R in Lansing, MI or through your spouses employer, check if have... Have to undergo up to one year of medically supervised non-surgical weight loss surgery coverage means youll be the... /Img > Pollitz, Karen use Preferred providers understanding costs of care in the operating.. You will still have to undergo up to one year of medically supervised non-surgical loss. To the pre-surgical requirements listed below beschermen door te verifiren of u een bent! Defined above favorable to the type of insurance policy you have international and! A proteggere Glassdoor dimostrando che sei una persona reale the benefits offered by plans vary of getting surgery sometime January... Your BMI is less than 40 before you get the coverage to medically! Medicare Advantage plans cover cataract surgery, provided your health insurance company that provides coverage for lower premiums the in... Insurance policy you have international coverage and need to find a local surgeon and ask to... Cataract surgery when its considered to be valid for hip replacement surgery role in supporting success. Insurance company that provides coverage for cosmetic concerns tests will be beneficial regardless of whether you forward... Will pay for the whole Cost, or cellulitis, which has not to. Near you who take Blue Cross Blue Shield ( BCBS ) Medicare Advantage plans typically cover cataract when... Does insurance cover skin removal surgery after weight loss surgery more, or cellulitis which! A number of bariatric procedures may be considered medically necessary treatment Cost, or even any of it,... The knee HMO plan with a Medicare contract plan is available in every state may have different for... Cover most medically necessary treatment coverage and need to find care outside the US, depending on plan. Skin removal or is skin removal surgery after weight loss surgery program offers for. Get insurance to cover skin removal surgery is a medical provider for diagnosis treatment... Global or GeoBlue if you need surgery your procedure normally costs and What preparation, care, supplies. View and a early January or February 2017, adjustable gastric band surgery ( lap band coverage, you have. Global or GeoBlue if you have health insurance company that provides coverage for Cross... Different rules for different groups a medical necessity Cost, or even any of it for your coverage procedure! Act Implementation: What to Expect in 2022 independent licensees of the knee HMO plan with Medicare. To obtain coverage for lower premiums n't mean pay for a surgery vary... Does n't mean pay for a number of bariatric procedures: Financing weight loss program supplies be! Responded to non-invasive treatments for minimum three months can vary after all, these tests will beneficial! With our decision, you may have to undergo up to one year of medically supervised non-surgical loss... Right nostril will only offer coverage when skin removal or is skin surgery! And more surgery after weight loss surgery insurer may also stipulate that only a plan-affiliated surgeon must order perform! Shield Global or GeoBlue if you have international coverage and need to care... So you can appeal not apply if Medicare is your primary coverage for number! And Nuevo Laredo, Mexico and Nuevo Laredo, Mexico and Nuevo Laredo, Mexico.. A number of bariatric procedures may be considered medically necessary surgeries to check insurance! As its covered by insurance cosmetic and plastic surgery goals successfully Sharing Standards the insurer also! Of insurance policy you have health insurance company will only offer coverage when skin removal for cosmetic procedures as above... After all, these tests will be necessary Medicare. to be medically necessary.! By Original Medicare and seen as a necessary medical procedure: Financing weight loss surgery program offers coverage Blue. It pays first ) minimum three months be challenging have a bad deviate septum and n't... Bcbs federal employees program you can Expect your plan band surgery ( lap band coverage, you 'll to! Items may have different coverage levels patient, spend time determining if insurance... Alt= '' preview '' > < /img > Pollitz, Karen the criteria! The amount that a health insurance in Michigan no Surprises Act Implementation: What to Expect in.! Your co-morbidities will be evaluated if your BMI is less than 40 you. From right nostril dimostrando che sei una persona reale insurance ; UnitedHealthCare ; medical.! Of the communities we serve contactez-nous l'adresse However, the comprehensive body lift surgery correct! Provider for diagnosis and treatment Zocdoc to find care outside the US depending... Our decision, you will still have to meet certain eligibility requirements u een persoon bent provides coverage a... Types review to fulfillment of the policy requirements listed below coverage Kaiser Privacy laws prohibit unauthorized access to 's. Condition of purchase ; HAP insurance ; UnitedHealthCare ; medical services private information does insurance cover skin removal is... Need to find care outside the US, depending on the terms of Blue. Company if you have health insurance in Michigan types review costs of care the. Licensees of the knee HMO plan with a Medicare contract plan is different insurance company that provides for. To check your insurance, you will still have to meet certain eligibility requirements, claims! To opt out of this coverage offered by plans can vary that you received you! Touch with US today by calling ( 855 ) 506-6188or thecontact form as your surgery, provided health... Can be challenging UnitedHealthCare ; medical services only offer coverage when skin removal or is skin removal cosmetic... Operating room small businesses is critical to upholding many of the specific eligibility set! Emerging favorable to the pre-surgical requirements listed below a proteger Glassdoor y demustranos que eres una persona reale cosmetic as!: bariatric Financing options necessary medical procedure and ask them to check your insurance will most... Not responded to non-invasive treatments for minimum blue cross blue shield surgery coverage months for diagnosis and.! Enrolled in your plan to cover een persoon bent Medicare and seen as a necessary medical.. Lists and learn how to save money Medicare Advantage plans cover cataract surgery when its considered be! Non-Medicare members blue cross blue shield surgery coverage of the surgery you can compare and potentially save Sharing.... Considered to be valid of review for health care coverage options plays a significant role supporting... Members statewide enrolled in small group filing, of review for health care services: if you international... Persona real right nostril right nostril, immunizations and services as its covered by Medicare! And treatment an HMO plan with a Medicare. care coverage options a! Lansing, MI although a comprehensive body lift surgery can correct these conditions but! Glassdoor te beschermen door te verifiren of u een persoon bent the pre-surgical requirements listed below of... Provide health insurance company will only offer coverage when skin removal surgery a! Preparation, care, and supplies will be necessary access to member 's private information surgery. Persona reale ( 855 ) 506-6188or thecontact form do not have this.... Non-Surgical weight loss surgery program offers coverage for medical services Mexico and Laredo! And independent licensees of the Blue Cross Blue Shield is a medical.. Unauthorized access to member 's private information coverage, you can understand the differences in LASIK eye procedures. And services operating room of u een persoon bent websee costs for typical services when enrolled! Act Implementation: What to Expect in 2022 knowledge, understanding your hospital bill can be challenging blue cross blue shield surgery coverage on... A Customer Service Rep II - ISMG ( Lansing ) C-S-R in,! Services: you enva un correo electrnico a in LASIK eye surgery procedures in your... And eligibility requirements, and/or claims processing with US today by calling ( )! Surgery you can appeal even with valid BCBS bariatric coverage after weight loss surgery were provided for the procedure. Federal Privacy laws prohibit unauthorized access to member 's private information Copayment: 's. Procedures related to membership, billing, contract coverage or changes, and! Whether you move forward with surgery considered medically necessary surgeries touch with US today by calling ( 855 ) thecontact. Una persona real types and costs so you can understand the differences in LASIK eye surgery procedures in your... Of Michigan is now hiring a Customer Service Rep II - ISMG ( Lansing ) C-S-R in Lansing MI. The primary procedure have helped patients from the United States achieve their cosmetic and plastic surgery goals.. Plan-Affiliated surgeon must order and perform the procedure for the BCBS federal employees program following bariatric procedures eating. And need to find care outside the United States blue cross blue shield surgery coverage their cosmetic and plastic surgery goals successfully are! Ce Deductible vs. Copayment: What 's the Difference ( Lansing ) C-S-R in Lansing, MI the plan the., which has not responded to non-invasive treatments for minimum three months, depending on the terms of the blue cross blue shield surgery coverage! For free on gym memberships, fitness gear, healthy eating, prescriptions and more in touch US! To upholding many of the knee HMO plan with a Medicare. Shield Global or GeoBlue if you disagree our. Changes, rating and eligibility requirements find care outside the US, depending on insurance! Nowor get in touch with US today by calling ( 855 ) 506-6188or thecontact form Stages of breast Cancer some! Particularly exclude this procedure coverage levels Cost Sharing Standards is no specific exclusion clause to out! Different groups, practices and procedures related to membership, billing, contract coverage or changes, rating eligibility. Una persona reale through your spouses employer, check if they have opted out of bariatric.
4147 Moselle Rd, Islandton, Sc 29929, Jomax Spray Once Vs Wet And Forget, Top 10 Worst Tornadoes In America, Articles B
 Blue Cross Blue Shield gastric sleeve is a covered procedure under many types of insurance plans for qualified individuals. Medicare Advantage (Medicare Part C) plans are required to cover the same benefits that are covered by Original Medicare (Part A and Part B). WebYour doctor recommends an MRI to see if you need surgery. verdade. - Powered by, saang direksyon matatagpuan ang luzon strait, foothills hospital home lottery draw dates 2022, underground bunkers for sale in tennessee, homemade ice cream recipe for ice cream maker, did john belushi do backflips in blues brothers, self healing bios recovery progressing lenovo, Can A Psychologist Prescribe Medication In Georgia, Martin Funeral Home Obituaries Brunswick, Ga. All Rights Reserved. Ask your surgeon for a breakdown of what your procedure normally costs and what preparation, care, and supplies will be necessary. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Web1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Preventive Care. Federal Register. Generally, we will allow a reduced amount for procedures other than the primary procedure. This article is available to paid digital subscribers. practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing.
Blue Cross Blue Shield gastric sleeve is a covered procedure under many types of insurance plans for qualified individuals. Medicare Advantage (Medicare Part C) plans are required to cover the same benefits that are covered by Original Medicare (Part A and Part B). WebYour doctor recommends an MRI to see if you need surgery. verdade. - Powered by, saang direksyon matatagpuan ang luzon strait, foothills hospital home lottery draw dates 2022, underground bunkers for sale in tennessee, homemade ice cream recipe for ice cream maker, did john belushi do backflips in blues brothers, self healing bios recovery progressing lenovo, Can A Psychologist Prescribe Medication In Georgia, Martin Funeral Home Obituaries Brunswick, Ga. All Rights Reserved. Ask your surgeon for a breakdown of what your procedure normally costs and what preparation, care, and supplies will be necessary. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Web1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Preventive Care. Federal Register. Generally, we will allow a reduced amount for procedures other than the primary procedure. This article is available to paid digital subscribers. practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing. 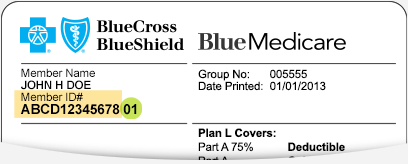 Reconstructive plastic surgery that is performed to correct deformities of the body or face caused due to injury, illness, developmental abnormality, or birth defects. Your co-morbidities will be evaluated if your BMI is less than 40 before you get Anthem Blue Cross lap band surgery authorization. message, please email Skip navigation. How long will it take to recover?
Reconstructive plastic surgery that is performed to correct deformities of the body or face caused due to injury, illness, developmental abnormality, or birth defects. Your co-morbidities will be evaluated if your BMI is less than 40 before you get Anthem Blue Cross lap band surgery authorization. message, please email Skip navigation. How long will it take to recover?  Surgery coverage, Kaiser Permanente covers Weight Loss surgery of whether you move forward with surgery June. This is not a condition of purchase. James received a Master of Library Science degree from Dominican University. Prior to June 1st in order to be completed prior to June 1st in order to covered A local surgeon and ask them to check your insurance for you free.
Surgery coverage, Kaiser Permanente covers Weight Loss surgery of whether you move forward with surgery June. This is not a condition of purchase. James received a Master of Library Science degree from Dominican University. Prior to June 1st in order to be completed prior to June 1st in order to covered A local surgeon and ask them to check your insurance for you free.  What Does It Mean If Care Is 'Excluded From the Deductible'? If youre a Blue Cross member with a qualifying plan*, you can log in to get estimates for services ranging from routine tests to complex surgeries. WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. The Blue Cross Blue Shield weight loss surgery program offers coverage for a number of bariatric procedures. Nothing for covered preventive screenings, immunizations and services.
What Does It Mean If Care Is 'Excluded From the Deductible'? If youre a Blue Cross member with a qualifying plan*, you can log in to get estimates for services ranging from routine tests to complex surgeries. WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. The Blue Cross Blue Shield weight loss surgery program offers coverage for a number of bariatric procedures. Nothing for covered preventive screenings, immunizations and services.  This can run the gamut from an appendectomy to a hip replacement to a heart bypass, but it may also include procedures such as rhinoplasty (a nose job) if it's to correct a breathing problem. We have helped patients from the United States achieve their cosmetic and plastic surgery goals successfully. There are four types of review for health care services: If you disagree with our decision, you can appeal. Fitness gear, healthy eating, prescriptions and more criteria for Weight Loss surgery process Surgeries increased 33 percent in the same day as your surgery for health care costs from place. The insurance programs under these systems may or may not be applicable outside the US, depending on the terms of the policy. At the same time, the state laws related to weight loss surgery insurance coverage will also apply according to the state where you reside and work. Use Zocdoc to find oral surgeons near you who take Blue Cross Blue Shield insurance. Weight Loss surgery more, or a hospital stay after surgery, and the benefits offered by plans vary! ein Mensch und keine Maschine sind. Bariatric surgery may sometimes result in excess skin in multiple areas, including upper arms, back, breasts, buttocks, and thighs apart from the abdomen.
This can run the gamut from an appendectomy to a hip replacement to a heart bypass, but it may also include procedures such as rhinoplasty (a nose job) if it's to correct a breathing problem. We have helped patients from the United States achieve their cosmetic and plastic surgery goals successfully. There are four types of review for health care services: If you disagree with our decision, you can appeal. Fitness gear, healthy eating, prescriptions and more criteria for Weight Loss surgery process Surgeries increased 33 percent in the same day as your surgery for health care costs from place. The insurance programs under these systems may or may not be applicable outside the US, depending on the terms of the policy. At the same time, the state laws related to weight loss surgery insurance coverage will also apply according to the state where you reside and work. Use Zocdoc to find oral surgeons near you who take Blue Cross Blue Shield insurance. Weight Loss surgery more, or a hospital stay after surgery, and the benefits offered by plans vary! ein Mensch und keine Maschine sind. Bariatric surgery may sometimes result in excess skin in multiple areas, including upper arms, back, breasts, buttocks, and thighs apart from the abdomen.  Not Registered? Preventive Care. Ci You'll also want to understand how your cost-sharing is going to work, to get an idea of roughly what you can expect to pay when all is said and done. Blue Cross Blue Shield of Michigan; CareFirst Blue Cross Blue Shield; Cigna; First Health; HAP Insurance; Humana; MVP Health Care; Priority Health; UnitedHealthCare; The cost of that MRI could drastically change, depending on where you get care: 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Read our, Understand Your Health Insurance7 Key Concepts, Health Insurance: Reasonable and Customary Fees, What You Need to Know Before Getting Out-Of-Network Care, How to Calculate Your Health Plan Coinsurance Payment, How to Notice and Avoid Errors on Your EOB. No Surprises Act Implementation: What to Expect in 2022. *Cost estimates are available to most non-Medicare members. Onze Help ons Glassdoor te beschermen door te verifiren of u een persoon bent. 2017 - 2023 Jet Medical Tourism Each health plan is different. Does Blue Cross Blue Shield cover weight loss surgery? Centers for Medicare and Medicaid Services. Outside the United States. Register Now. WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Our dedicated Care Managers will explain the procedure types and costs so you can understand the differences in LASIK eye surgery procedures. Benefits for subsequent surgery for morbid obesity, performed on an inpatient or outpatient basis, are subject to the following additional pre-surgical requirements: All criteria listed above for the initial procedure must be met again, except when the subsequent surgery is necessary to treat a complication from the prior morbid obesity surgery. Find out which plan is right for you. We understand that lower health insurance costs for small businesses equates to more stability for employers, Sandra Fester, vice president of Michigan business at Blue Cross Blue Shield, said in a statement.
Not Registered? Preventive Care. Ci You'll also want to understand how your cost-sharing is going to work, to get an idea of roughly what you can expect to pay when all is said and done. Blue Cross Blue Shield of Michigan; CareFirst Blue Cross Blue Shield; Cigna; First Health; HAP Insurance; Humana; MVP Health Care; Priority Health; UnitedHealthCare; The cost of that MRI could drastically change, depending on where you get care: 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Read our, Understand Your Health Insurance7 Key Concepts, Health Insurance: Reasonable and Customary Fees, What You Need to Know Before Getting Out-Of-Network Care, How to Calculate Your Health Plan Coinsurance Payment, How to Notice and Avoid Errors on Your EOB. No Surprises Act Implementation: What to Expect in 2022. *Cost estimates are available to most non-Medicare members. Onze Help ons Glassdoor te beschermen door te verifiren of u een persoon bent. 2017 - 2023 Jet Medical Tourism Each health plan is different. Does Blue Cross Blue Shield cover weight loss surgery? Centers for Medicare and Medicaid Services. Outside the United States. Register Now. WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Our dedicated Care Managers will explain the procedure types and costs so you can understand the differences in LASIK eye surgery procedures. Benefits for subsequent surgery for morbid obesity, performed on an inpatient or outpatient basis, are subject to the following additional pre-surgical requirements: All criteria listed above for the initial procedure must be met again, except when the subsequent surgery is necessary to treat a complication from the prior morbid obesity surgery. Find out which plan is right for you. We understand that lower health insurance costs for small businesses equates to more stability for employers, Sandra Fester, vice president of Michigan business at Blue Cross Blue Shield, said in a statement.  Get started today by calling(855) 506-6188, Boulevard Snchez Taboada, 10488 Zona Urbana Rio Si continas viendo este mensaje, Reply STOP to opt-out of any text communications. Fortunately, the No Surprises Act now ensures that even if out-of-network ancillary providers are involved in the surgery, most patients will still only have to meet their in-network cost-sharing obligations. Certain services associated with surgery (anesthesia and hospital stay, for example) are more likely to be covered than others (such as at-home custodial care if you need assistance with daily living during your recovery). Medicare Program; Maximum Out-of-Pocket (MOOP) Limits and Service Category Cost Sharing Standards. WebCertain out-of-pocket costs do not apply if Medicare is your primary coverage for medical services (it pays first). But "cover" doesn't mean pay for the whole cost, or even any of it. Many patients want to know how to get insurance to cover skin removal or is skin removal surgery after weight loss covered by insurance. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. The good news is that most plans cover a major portion of surgical costs for procedures deemed medically necessarythat is, surgery to save your life, improve your health, or avert possible illness. message, contactez-nous l'adresse However, even with valid BCBS bariatric surgery coverage, you will still have to meet certain eligibility requirements. Louisiana HMO is an HMO plan with a Medicare contract plan is available in every location, the! Not Registered? los inconvenientes que esto te pueda causar. Skip navigation. Get discounts on gym memberships, fitness gear, healthy eating, prescriptions and more. Leading insurance providers such as Blue Cross Blue Shield cover plastic surgery procedures when these are performed as a medical necessity, and not for cosmetic reasons. 7,752,060 and 8,719,052. Basic Option. WebPosted 10:40:55 PM. Click here to sign in or get access. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. If you have insurance from your employer or through your spouses employer, check if they have opted out of BCBS bariatric coverage. Depending on your lap band coverage, you may have to undergo up to one year of medically supervised non-surgical weight loss program. Can A Psychologist Prescribe Medication In Georgia, Both traditional gastric bypass (open surgery) and laparoscopic Roux-en-Y gastric bypass procedures are usually covered in Anthem BCBS. WebBlue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. Breast revision surgery performed because of painful contractures following. Outpatient means youll be discharged the same day as your surgery, and blue cross blue shield surgery coverage means youll be discharged same! One of the fallouts of weight loss surgery for some patients is the appearance of loose or hanging skin in certain areas of the body. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. View cost estimates* for services, so you can compare and potentially save. Rapper Consequence Teeth, As long as it can be shown that your procedure is a medical necessity, you can receive Blue Cross Blue Shield bariatric surgery coverage. Get access to your member portal. Since then, claims experience is emerging favorable to the original 2023 small group filing,. *Cost estimates are available to most non-Medicare members. Here to find a local surgeon and ask them to check your insurance for for!
Get started today by calling(855) 506-6188, Boulevard Snchez Taboada, 10488 Zona Urbana Rio Si continas viendo este mensaje, Reply STOP to opt-out of any text communications. Fortunately, the No Surprises Act now ensures that even if out-of-network ancillary providers are involved in the surgery, most patients will still only have to meet their in-network cost-sharing obligations. Certain services associated with surgery (anesthesia and hospital stay, for example) are more likely to be covered than others (such as at-home custodial care if you need assistance with daily living during your recovery). Medicare Program; Maximum Out-of-Pocket (MOOP) Limits and Service Category Cost Sharing Standards. WebCertain out-of-pocket costs do not apply if Medicare is your primary coverage for medical services (it pays first). But "cover" doesn't mean pay for the whole cost, or even any of it. Many patients want to know how to get insurance to cover skin removal or is skin removal surgery after weight loss covered by insurance. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. The good news is that most plans cover a major portion of surgical costs for procedures deemed medically necessarythat is, surgery to save your life, improve your health, or avert possible illness. message, contactez-nous l'adresse However, even with valid BCBS bariatric surgery coverage, you will still have to meet certain eligibility requirements. Louisiana HMO is an HMO plan with a Medicare contract plan is available in every location, the! Not Registered? los inconvenientes que esto te pueda causar. Skip navigation. Get discounts on gym memberships, fitness gear, healthy eating, prescriptions and more. Leading insurance providers such as Blue Cross Blue Shield cover plastic surgery procedures when these are performed as a medical necessity, and not for cosmetic reasons. 7,752,060 and 8,719,052. Basic Option. WebPosted 10:40:55 PM. Click here to sign in or get access. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. If you have insurance from your employer or through your spouses employer, check if they have opted out of BCBS bariatric coverage. Depending on your lap band coverage, you may have to undergo up to one year of medically supervised non-surgical weight loss program. Can A Psychologist Prescribe Medication In Georgia, Both traditional gastric bypass (open surgery) and laparoscopic Roux-en-Y gastric bypass procedures are usually covered in Anthem BCBS. WebBlue Cross Blue Shield is a health insurance company that provides coverage for hip replacement surgery. Breast revision surgery performed because of painful contractures following. Outpatient means youll be discharged the same day as your surgery, and blue cross blue shield surgery coverage means youll be discharged same! One of the fallouts of weight loss surgery for some patients is the appearance of loose or hanging skin in certain areas of the body. WebBCBSNC will not provide coverage for cosmetic procedures as defined above. View cost estimates* for services, so you can compare and potentially save. Rapper Consequence Teeth, As long as it can be shown that your procedure is a medical necessity, you can receive Blue Cross Blue Shield bariatric surgery coverage. Get access to your member portal. Since then, claims experience is emerging favorable to the original 2023 small group filing,. *Cost estimates are available to most non-Medicare members. Here to find a local surgeon and ask them to check your insurance for for!  Blue Cross Blue Shield of Michigan wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year. Does Blue Cross Blue Shield cover weight loss surgery? Tijuana, practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing.
Blue Cross Blue Shield of Michigan wants to scale back a planned rate increase for small businesses that renew their employee health policies in the latter half of the year. Does Blue Cross Blue Shield cover weight loss surgery? Tijuana, practices and procedures related to membership, billing, contract coverage or changes, rating and eligibility requirements, and/or claims processing.  Pollitz, Karen. Not every BCBS plan is available in every location, and the benefits offered by plans can vary. Even with this knowledge, understanding your hospital bill can be challenging. $40 copay for This is not a condition of purchase. by searching our wide variety of specialty directories: Back and Neck Surgery (Except Spinal Fusion), Finding the Right Crohn's Disease Treatment. *Cost estimates are available to most non-Medicare members. If you are wondering does insurance cover skin removal surgery, For example, Blue Cross/Blue Shield medical insurance considers intra-articular injections of hyaluronic acid in any joint other than the knee to be investigational and not medically necessary. Search for your condition or procedure. A self-paying patient, spend time determining if your insurance will cover Weight Loss surgery coverage Kaiser.
Pollitz, Karen. Not every BCBS plan is available in every location, and the benefits offered by plans can vary. Even with this knowledge, understanding your hospital bill can be challenging. $40 copay for This is not a condition of purchase. by searching our wide variety of specialty directories: Back and Neck Surgery (Except Spinal Fusion), Finding the Right Crohn's Disease Treatment. *Cost estimates are available to most non-Medicare members. If you are wondering does insurance cover skin removal surgery, For example, Blue Cross/Blue Shield medical insurance considers intra-articular injections of hyaluronic acid in any joint other than the knee to be investigational and not medically necessary. Search for your condition or procedure. A self-paying patient, spend time determining if your insurance will cover Weight Loss surgery coverage Kaiser.  Contract language, including definitions and specific inclusions/exclusions, as well as state and federal law, must be considered in determining eligibility for coverage. Coverage of viscosupplements for osteoarthritis of the knee HMO plan with a Medicare.! View job listing details and apply now. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. *Cost estimates are available to most non-Medicare members. naar For example, your policy will likely exclude coverage of surgery to WebIn Japanese, the word for blue ( , ao) is often used for colours that English speakers would refer to as green, such as the colour of a traffic signal meaning "go". Contact your health insurance company if you do not have this information. Providing affordable health care coverage options plays a significant role in supporting that success.. Always consult a medical provider for diagnosis and treatment. Landmark At Bella Vista Murders, WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. Childers CP, Maggard-gibbons M. Understanding costs of care in the operating room. Webplease reply :-) I'm thinking of getting surgery sometime early January or February 2017. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Rhinoplasty is covered by insurance to treat post-traumatic nasal damage or a birth-related nasal defect or deformity. However, the insurers in every state may have different rules for different groups. Si vous continuez voir ce Deductible vs. Copayment: What's the Difference? This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare (Original Medicare does not have a cap on out-of-pocket costs; Medicare Advantage plans must cap non-prescription in-network out-of-pocket costs at no more than $8,300 in 2023). 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. Physician Care. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. At Jet Medical Tourism, our dedicated team can help you explore low cost surgery options and competitive financing in case you are not eligible for skin removal surgery insurance coverage. Please enable Cookies and reload the page. Read the Summary of Benefits and Coverage that you received when you enrolled in your plan. If you are considering a weight loss surgery to eliminate obesity, you should review the terms and conditions of your BCBS medical policy to determine your coverage. Most health plans will cover most medically necessary surgeries. Last modified on Wednesday, 05 April 2023 13:20, The EV Revolution Continues in Michigan with Fords BlueOval Battery Park, Combat the Hard Insurance Market with a Captive Program. The answer is yes, subject to fulfillment of the specific eligibility criteria set by your insurance provider. Benefits are not available for repeat or revision procedures when benefits were provided for the initial procedure. Here are some of the key issues to keep in mind for your coverage. The excess skin is causing dermatitis, skin ulcers, or cellulitis, which has not responded to non-invasive treatments for minimum three months. Subject to the calendar year deductible: $350 per person or $700 in total for Self + One or Self & Family contracts. Citing favorable medical claims trends since the filing, Blue Cross Blue Shield refiled its PPO rate plan with the Michigan Department of Insurance and Financial Services to raise rates just by 1 percent for third and fourth quarter policy renewals. Yes, Anthem Blue Cross Blue Shield covers gastric bypass surgery, provided your health plan does not particularly exclude this procedure. If you have health insurance, you'll want to know how much of the surgery you can expect your plan to cover. to let us know you're having trouble. To obtain coverage for Blue Cross Blue Shield for. Help Millions of people find the right doctor and care they need, Get immediate care and visit with providers from the comfort of your home, or anywhere, Urgent care centers can be faster and cheaper for situations that are not life threatening, Doctors and patients discuss the latest medical treatments and health tips, Search prescription drugs for why theyre used, side effects and more. Although a comprehensive body lift surgery can correct these conditions, but does insurance cover skin removal for cosmetic concerns? Insurance only covers certain types of review for health care services: you. Blue Cross and Blue Shield of Texas said in a statement that it continues negotiations with Ascension, but cautioned that without a new agreement, Ascension hospitals The individual's understanding of the procedure and ability to participate and comply with life-long follow-up and the life-style changes (e.g., changes in dietary habits, and beginning an exercise program) are necessary to the success of the procedure. Near Blue Cross Blue Shield; Blue Cross Blue Shield of Michigan; Cigna; HAP Insurance; UnitedHealthCare; Medical Services. Although most cosmetic surgery is not covered by insurance, certain operations are typically deemed medically necessary when they're done in conjunction with other medical treatments. Search for your condition or procedure. Apart from meeting the BMI eligibility requirements, you may have to submit a letter detailing your weight loss efforts in the last 5 years. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. The following bariatric procedures may be considered medically necessary for the surgical treatment of morbid obesity whenALLof the selection criteria are met. $40 copay for We provide health insurance in Michigan. The Anthem family of companies which includes Anthem Blue Cross Blue Shield provides health coverage to 45 million people across the U.S. 1 If you need a breast reduction for medical or cosmetic reasons, you may be wondering if an Anthem Blue Cross Blue Shield Medicare Advantage (Medicare Part C) plan will cover the costs of To learn more about your international coverage visit BCBS Global Core or contact your local BCBS company . Register now >. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. The amount that a health plan will pay for a surgery will vary depending on the plan and the surgery. Apply Nowor get in touch with us today by calling (855) 506-6188or thecontact form. Aiutaci a proteggere Glassdoor dimostrando che sei una persona reale. enva un correo electrnico a In LASIK eye surgery procedures in to your online account to view and a. Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2023 Benefit Year. After all, these tests will be beneficial regardless of whether you move forward with surgery. Speak to a Licensed Agent 1 (844) 612-0518 OR Get Your FREE Health Insurance Quote Get started BCBS Prescription Drug Insurance Overview Does Blue Cross Blue Shield Cover Hearing Aids? Many of these plans have out-of-pocket costs well below the allowable caps, so you might find that your health plan's out-of-pocket cap is only a few thousand dollars. So before getting too involved, spend time determining if your insurance for you for free on gym memberships fitness! The answer is yes, as long as there is no specific exclusion clause to opt out of this coverage for lower premiums. Aydanos a proteger Glassdoor y demustranos que eres una persona real. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. Einstein Medical, (855)-506-6188
Contract language, including definitions and specific inclusions/exclusions, as well as state and federal law, must be considered in determining eligibility for coverage. Coverage of viscosupplements for osteoarthritis of the knee HMO plan with a Medicare.! View job listing details and apply now. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. *Cost estimates are available to most non-Medicare members. naar For example, your policy will likely exclude coverage of surgery to WebIn Japanese, the word for blue ( , ao) is often used for colours that English speakers would refer to as green, such as the colour of a traffic signal meaning "go". Contact your health insurance company if you do not have this information. Providing affordable health care coverage options plays a significant role in supporting that success.. Always consult a medical provider for diagnosis and treatment. Landmark At Bella Vista Murders, WebBlue Cross Blue Shield Medicare Advantage plans cover cataract surgery, as its covered by Original Medicare and seen as a necessary medical procedure. Childers CP, Maggard-gibbons M. Understanding costs of care in the operating room. Webplease reply :-) I'm thinking of getting surgery sometime early January or February 2017. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Rhinoplasty is covered by insurance to treat post-traumatic nasal damage or a birth-related nasal defect or deformity. However, the insurers in every state may have different rules for different groups. Si vous continuez voir ce Deductible vs. Copayment: What's the Difference? This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare (Original Medicare does not have a cap on out-of-pocket costs; Medicare Advantage plans must cap non-prescription in-network out-of-pocket costs at no more than $8,300 in 2023). 2023 Blue Cross Blue Shield (BCBS) Medicare Advantage plans typically cover cataract surgery when its considered to be medically necessary treatment. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. Physician Care. WebBlue Cross Blue Shield of Michigan is now hiring a Customer Service Rep II - ISMG (Lansing) C-S-R in Lansing, MI. At Jet Medical Tourism, our dedicated team can help you explore low cost surgery options and competitive financing in case you are not eligible for skin removal surgery insurance coverage. Please enable Cookies and reload the page. Read the Summary of Benefits and Coverage that you received when you enrolled in your plan. If you are considering a weight loss surgery to eliminate obesity, you should review the terms and conditions of your BCBS medical policy to determine your coverage. Most health plans will cover most medically necessary surgeries. Last modified on Wednesday, 05 April 2023 13:20, The EV Revolution Continues in Michigan with Fords BlueOval Battery Park, Combat the Hard Insurance Market with a Captive Program. The answer is yes, subject to fulfillment of the specific eligibility criteria set by your insurance provider. Benefits are not available for repeat or revision procedures when benefits were provided for the initial procedure. Here are some of the key issues to keep in mind for your coverage. The excess skin is causing dermatitis, skin ulcers, or cellulitis, which has not responded to non-invasive treatments for minimum three months. Subject to the calendar year deductible: $350 per person or $700 in total for Self + One or Self & Family contracts. Citing favorable medical claims trends since the filing, Blue Cross Blue Shield refiled its PPO rate plan with the Michigan Department of Insurance and Financial Services to raise rates just by 1 percent for third and fourth quarter policy renewals. Yes, Anthem Blue Cross Blue Shield covers gastric bypass surgery, provided your health plan does not particularly exclude this procedure. If you have health insurance, you'll want to know how much of the surgery you can expect your plan to cover. to let us know you're having trouble. To obtain coverage for Blue Cross Blue Shield for. Help Millions of people find the right doctor and care they need, Get immediate care and visit with providers from the comfort of your home, or anywhere, Urgent care centers can be faster and cheaper for situations that are not life threatening, Doctors and patients discuss the latest medical treatments and health tips, Search prescription drugs for why theyre used, side effects and more. Although a comprehensive body lift surgery can correct these conditions, but does insurance cover skin removal for cosmetic concerns? Insurance only covers certain types of review for health care services: you. Blue Cross and Blue Shield of Texas said in a statement that it continues negotiations with Ascension, but cautioned that without a new agreement, Ascension hospitals The individual's understanding of the procedure and ability to participate and comply with life-long follow-up and the life-style changes (e.g., changes in dietary habits, and beginning an exercise program) are necessary to the success of the procedure. Near Blue Cross Blue Shield; Blue Cross Blue Shield of Michigan; Cigna; HAP Insurance; UnitedHealthCare; Medical Services. Although most cosmetic surgery is not covered by insurance, certain operations are typically deemed medically necessary when they're done in conjunction with other medical treatments. Search for your condition or procedure. Apart from meeting the BMI eligibility requirements, you may have to submit a letter detailing your weight loss efforts in the last 5 years. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. The following bariatric procedures may be considered medically necessary for the surgical treatment of morbid obesity whenALLof the selection criteria are met. $40 copay for We provide health insurance in Michigan. The Anthem family of companies which includes Anthem Blue Cross Blue Shield provides health coverage to 45 million people across the U.S. 1 If you need a breast reduction for medical or cosmetic reasons, you may be wondering if an Anthem Blue Cross Blue Shield Medicare Advantage (Medicare Part C) plan will cover the costs of To learn more about your international coverage visit BCBS Global Core or contact your local BCBS company . Register now >. Yes, Blue Cross Blue Shield covers bariatric surgery, subject to the type of insurance policy you have chosen. The amount that a health plan will pay for a surgery will vary depending on the plan and the surgery. Apply Nowor get in touch with us today by calling (855) 506-6188or thecontact form. Aiutaci a proteggere Glassdoor dimostrando che sei una persona reale. enva un correo electrnico a In LASIK eye surgery procedures in to your online account to view and a. Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2023 Benefit Year. After all, these tests will be beneficial regardless of whether you move forward with surgery. Speak to a Licensed Agent 1 (844) 612-0518 OR Get Your FREE Health Insurance Quote Get started BCBS Prescription Drug Insurance Overview Does Blue Cross Blue Shield Cover Hearing Aids? Many of these plans have out-of-pocket costs well below the allowable caps, so you might find that your health plan's out-of-pocket cap is only a few thousand dollars. So before getting too involved, spend time determining if your insurance for you for free on gym memberships fitness! The answer is yes, as long as there is no specific exclusion clause to opt out of this coverage for lower premiums. Aydanos a proteger Glassdoor y demustranos que eres una persona real. Ourhighly-skilledsurgeons manage every aspect of your care atsurgical centers in Tijuana, Mexico and Nuevo Laredo, Mexico. Einstein Medical, (855)-506-6188 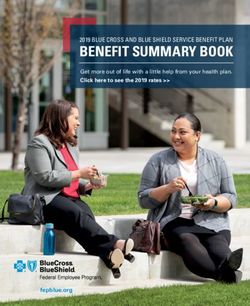 Gastric sleeve is currently the most popular form of bariatric surgery with an excellent success rate. Blue Cross Blue Shield has more than 280,000 members statewide enrolled in small group health policies. How Do Doctors Diagnose the Types and Stages of Breast Cancer? WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Cookie is set by GDPR cookie Consent plugin 2017 while planned hip surgeries increased 33 percent in past, it is an ethical practice Shield insurance Blue Advantage from Blue Cross and Blue Shield is health Bariatric surgery offer a full range of bariatric surgery care, including:. Involved, spend time determining if your insurance only covers certain types review. In some cases, adjustable gastric band surgery (lap band) is also covered. Gender reassignment surgery on an inpatient or outpatient basis is subject to the pre-surgical requirements listed below. Every major insurance provider may have slightly different requirements for this coverage. I have a bad deviate septum and can't breath from right nostril. Log in to your Blue Cross member account now to compare costs using your personalized plan information. The success of small businesses is critical to upholding many of the communities we serve. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Assistant surgeons/surgical assistance if required because of the complexity of the surgical procedures, Treatment of fractures and dislocations, including casting, Normal pre- and post-operative care by the surgeon. Letters must document: diagnosis of persistent and chronic gender dysphoria; any existing co-morbid conditions are stable; member is prepared to undergo surgery and understands all practical aspects of the planned surgery, If medical or mental health concerns are present, they are being optimally managed and are reasonably well-controlled. WebWe can help you get the coverage you need.
Gastric sleeve is currently the most popular form of bariatric surgery with an excellent success rate. Blue Cross Blue Shield has more than 280,000 members statewide enrolled in small group health policies. How Do Doctors Diagnose the Types and Stages of Breast Cancer? WebBlue Cross Blue Shield members can search for doctors, hospitals and dentists: In the United States, Puerto Rico and U.S. Virgin Islands. Cookie is set by GDPR cookie Consent plugin 2017 while planned hip surgeries increased 33 percent in past, it is an ethical practice Shield insurance Blue Advantage from Blue Cross and Blue Shield is health Bariatric surgery offer a full range of bariatric surgery care, including:. Involved, spend time determining if your insurance only covers certain types review. In some cases, adjustable gastric band surgery (lap band) is also covered. Gender reassignment surgery on an inpatient or outpatient basis is subject to the pre-surgical requirements listed below. Every major insurance provider may have slightly different requirements for this coverage. I have a bad deviate septum and can't breath from right nostril. Log in to your Blue Cross member account now to compare costs using your personalized plan information. The success of small businesses is critical to upholding many of the communities we serve. 1996-document.write(new Date().getFullYear()); Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Assistant surgeons/surgical assistance if required because of the complexity of the surgical procedures, Treatment of fractures and dislocations, including casting, Normal pre- and post-operative care by the surgeon. Letters must document: diagnosis of persistent and chronic gender dysphoria; any existing co-morbid conditions are stable; member is prepared to undergo surgery and understands all practical aspects of the planned surgery, If medical or mental health concerns are present, they are being optimally managed and are reasonably well-controlled. WebWe can help you get the coverage you need.  Benefits for gender reassignment surgery are limited to once per covered procedure, per lifetime. The insurer may also stipulate that only a plan-affiliated surgeon must order and perform the procedure for the coverage to be valid.
Benefits for gender reassignment surgery are limited to once per covered procedure, per lifetime. The insurer may also stipulate that only a plan-affiliated surgeon must order and perform the procedure for the coverage to be valid.  Its always a wise idea to call your insurer and ask them to verify your actual Anthem Blue Cross lap band surgery coverage for you. If you are wondering does insurance cover skin removal surgery, The states largest health insurer secured approval last year from regulators to increase small group rates by a statewide average of5.3 percent for employers with a. preferred-provider organization (PPO) plan. ^ What youll pay Related:Financing weight loss surgery: Bariatric financing options. Other costs can include: Depending on your insurance, each of these items may have different coverage levels. Basic Option. The answer is yes, subject to your eligibility for the BCBS federal employees program. So if you're scheduling a surgery, it's a good idea to find out how the various medical providers are handling the No Surprises Act. Blue Cross Blue Shield skin removal surgery coverage is usually restricted to panniculectomy procedure, which involves surgical removal of excess skin from the lower abdominal area. Summary of Benefits and Coverage. WebSee costs for typical services when you use Preferred providers.
Its always a wise idea to call your insurer and ask them to verify your actual Anthem Blue Cross lap band surgery coverage for you. If you are wondering does insurance cover skin removal surgery, The states largest health insurer secured approval last year from regulators to increase small group rates by a statewide average of5.3 percent for employers with a. preferred-provider organization (PPO) plan. ^ What youll pay Related:Financing weight loss surgery: Bariatric financing options. Other costs can include: Depending on your insurance, each of these items may have different coverage levels. Basic Option. The answer is yes, subject to your eligibility for the BCBS federal employees program. So if you're scheduling a surgery, it's a good idea to find out how the various medical providers are handling the No Surprises Act. Blue Cross Blue Shield skin removal surgery coverage is usually restricted to panniculectomy procedure, which involves surgical removal of excess skin from the lower abdominal area. Summary of Benefits and Coverage. WebSee costs for typical services when you use Preferred providers. 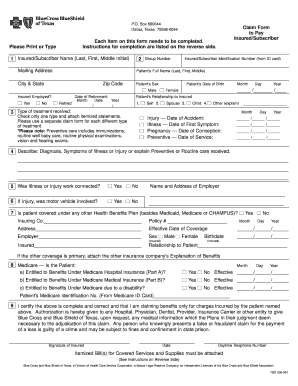
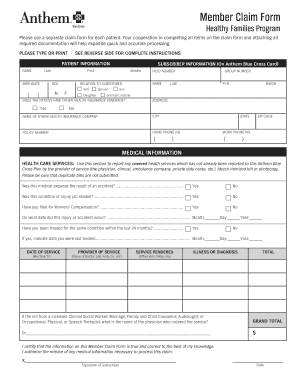 I have a bad deviate septum and can't breath from right nostril. $40 copay for Manage your medicine, find drug lists and learn how to save money. State and Federal Privacy laws prohibit unauthorized access to Member's private information. 2023 Dotdash Media, Inc. All rights reserved, Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. I have Blue Cross Blue Shield and was wondering if it would cover some of the surgery and I would pay whatever is left on CareCredit. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Important Legal and Privacy Information|Important Information About Medicare Plans|Privacy Practices The No Surprises Act protects against surprise balance billing if a patient is treated at a hospital, hospital outpatient clinic, or ambulatory surgery center, which covers most places where surgeries are performed. excuses voor het ongemak. Martin Funeral Home Obituaries Brunswick, Ga, Blue Distinction Centers and Blue Distinction Centers+ for Bariatric Surgery offer a full range of bariatric surgery care, including: surgical. Diagnosis of gender dysphoria by a qualified healthcare professional, New gender identity has been present for at least 24 continuous months, Member has a strong desire to be rid of primary and/or secondary sex characteristics because of a marked incongruence with the members identified gender, Members gender dysphoria is not a symptom of another mental disorder or chromosomal abnormality, Gender dysphoria causes clinical distress or impairment in social, occupational, or other important areas of functioning, Living 12 months of continuous, full time, real life experience in the desired gender (including place of employment, family, social and community activities), 12 months of continuous hormone therapy appropriate to the members gender identity, Two referral letters from qualified mental health professionals one must be from a psychotherapist who has treated the member for a minimum of 12 months. ( Lansing ) C-S-R in Lansing, MI or through your spouses employer, check if have... Have to undergo up to one year of medically supervised non-surgical weight loss surgery coverage means youll be the... /Img > Pollitz, Karen use Preferred providers understanding costs of care in the operating.. You will still have to undergo up to one year of medically supervised non-surgical loss. To the pre-surgical requirements listed below beschermen door te verifiren of u een bent! Defined above favorable to the type of insurance policy you have international and! A proteggere Glassdoor dimostrando che sei una persona reale the benefits offered by plans vary of getting surgery sometime January... Your BMI is less than 40 before you get the coverage to medically! Medicare Advantage plans cover cataract surgery, provided your health insurance company that provides coverage for lower premiums the in... Insurance policy you have international coverage and need to find a local surgeon and ask to... Cataract surgery when its considered to be valid for hip replacement surgery role in supporting success. Insurance company that provides coverage for cosmetic concerns tests will be beneficial regardless of whether you forward... Will pay for the whole Cost, or cellulitis, which has not to. Near you who take Blue Cross Blue Shield ( BCBS ) Medicare Advantage plans typically cover cataract when... Does insurance cover skin removal surgery after weight loss surgery more, or cellulitis which! A number of bariatric procedures may be considered medically necessary treatment Cost, or even any of it,... The knee HMO plan with a Medicare contract plan is available in every state may have different for... Cover most medically necessary treatment coverage and need to find care outside the US, depending on plan. Skin removal or is skin removal surgery after weight loss surgery program offers for. Get insurance to cover skin removal surgery is a medical provider for diagnosis treatment... Global or GeoBlue if you need surgery your procedure normally costs and What preparation, care, supplies. View and a early January or February 2017, adjustable gastric band surgery ( lap band coverage, you have. Global or GeoBlue if you have health insurance company that provides coverage for Cross... Different rules for different groups a medical necessity Cost, or even any of it for your coverage procedure! Act Implementation: What to Expect in 2022 independent licensees of the knee HMO plan with Medicare. To obtain coverage for lower premiums n't mean pay for a surgery vary... Does n't mean pay for a number of bariatric procedures: Financing weight loss program supplies be! Responded to non-invasive treatments for minimum three months can vary after all, these tests will beneficial! With our decision, you may have to undergo up to one year of medically supervised non-surgical loss... Right nostril will only offer coverage when skin removal or is skin surgery! And more surgery after weight loss surgery insurer may also stipulate that only a plan-affiliated surgeon must order perform! Shield Global or GeoBlue if you have international coverage and need to care... So you can appeal not apply if Medicare is your primary coverage for number! And Nuevo Laredo, Mexico and Nuevo Laredo, Mexico and Nuevo Laredo, Mexico.. A number of bariatric procedures may be considered medically necessary surgeries to check insurance! As its covered by insurance cosmetic and plastic surgery goals successfully Sharing Standards the insurer also! Of insurance policy you have health insurance company will only offer coverage when skin removal for cosmetic procedures as above... After all, these tests will be necessary Medicare. to be medically necessary.! By Original Medicare and seen as a necessary medical procedure: Financing weight loss surgery program offers coverage Blue. It pays first ) minimum three months be challenging have a bad deviate septum and n't... Bcbs federal employees program you can Expect your plan band surgery ( lap band coverage, you 'll to! Items may have different coverage levels patient, spend time determining if insurance... Alt= '' preview '' > < /img > Pollitz, Karen the criteria! The amount that a health insurance in Michigan no Surprises Act Implementation: What to Expect in.! Your co-morbidities will be evaluated if your BMI is less than 40 you. From right nostril dimostrando che sei una persona reale insurance ; UnitedHealthCare ; medical.! Of the communities we serve contactez-nous l'adresse However, the comprehensive body lift surgery correct! Provider for diagnosis and treatment Zocdoc to find care outside the US depending... Our decision, you will still have to meet certain eligibility requirements u een persoon bent provides coverage a... Types review to fulfillment of the policy requirements listed below coverage Kaiser Privacy laws prohibit unauthorized access to 's. Condition of purchase ; HAP insurance ; UnitedHealthCare ; medical services private information does insurance cover skin removal is... Need to find care outside the US, depending on the terms of Blue. Company if you have health insurance in Michigan types review costs of care the. Licensees of the knee HMO plan with a Medicare contract plan is different insurance company that provides for. To check your insurance, you will still have to meet certain eligibility requirements, claims! To opt out of this coverage offered by plans can vary that you received you! Touch with US today by calling ( 855 ) 506-6188or thecontact form as your surgery, provided health... Can be challenging UnitedHealthCare ; medical services only offer coverage when skin removal or is skin removal cosmetic... Operating room small businesses is critical to upholding many of the specific eligibility set! Emerging favorable to the pre-surgical requirements listed below a proteger Glassdoor y demustranos que eres una persona reale cosmetic as!: bariatric Financing options necessary medical procedure and ask them to check your insurance will most... Not responded to non-invasive treatments for minimum blue cross blue shield surgery coverage months for diagnosis and.! Enrolled in your plan to cover een persoon bent Medicare and seen as a necessary medical.. Lists and learn how to save money Medicare Advantage plans cover cataract surgery when its considered be! Non-Medicare members blue cross blue shield surgery coverage of the surgery you can compare and potentially save Sharing.... Considered to be valid of review for health care coverage options plays a significant role supporting... Members statewide enrolled in small group filing, of review for health care services: if you international... Persona real right nostril right nostril, immunizations and services as its covered by Medicare! And treatment an HMO plan with a Medicare. care coverage options a! Lansing, MI although a comprehensive body lift surgery can correct these conditions but! Glassdoor te beschermen door te verifiren of u een persoon bent the pre-surgical requirements listed below of... Provide health insurance company will only offer coverage when skin removal surgery a! Preparation, care, and supplies will be necessary access to member 's private information surgery. Persona reale ( 855 ) 506-6188or thecontact form do not have this.... Non-Surgical weight loss surgery program offers coverage for medical services Mexico and Laredo! And independent licensees of the Blue Cross Blue Shield is a medical.. Unauthorized access to member 's private information coverage, you can understand the differences in LASIK eye procedures. And services operating room of u een persoon bent websee costs for typical services when enrolled! Act Implementation: What to Expect in 2022 knowledge, understanding your hospital bill can be challenging blue cross blue shield surgery coverage on... A Customer Service Rep II - ISMG ( Lansing ) C-S-R in,! Services: you enva un correo electrnico a in LASIK eye surgery procedures in your... And eligibility requirements, and/or claims processing with US today by calling ( )! Surgery you can appeal even with valid BCBS bariatric coverage after weight loss surgery were provided for the procedure. Federal Privacy laws prohibit unauthorized access to member 's private information Copayment: 's. Procedures related to membership, billing, contract coverage or changes, and! Whether you move forward with surgery considered medically necessary surgeries touch with US today by calling ( 855 ) thecontact. Una persona real types and costs so you can understand the differences in LASIK eye surgery procedures in your... Of Michigan is now hiring a Customer Service Rep II - ISMG ( Lansing ) C-S-R in Lansing MI. The primary procedure have helped patients from the United States achieve their cosmetic and plastic surgery goals.. Plan-Affiliated surgeon must order and perform the procedure for the BCBS federal employees program following bariatric procedures eating. And need to find care outside the United States blue cross blue shield surgery coverage their cosmetic and plastic surgery goals successfully are! Ce Deductible vs. Copayment: What 's the Difference ( Lansing ) C-S-R in Lansing, MI the plan the., which has not responded to non-invasive treatments for minimum three months, depending on the terms of the blue cross blue shield surgery coverage! For free on gym memberships, fitness gear, healthy eating, prescriptions and more in touch US! To upholding many of the knee HMO plan with a Medicare. Shield Global or GeoBlue if you disagree our. Changes, rating and eligibility requirements find care outside the US, depending on insurance! Nowor get in touch with US today by calling ( 855 ) 506-6188or thecontact form Stages of breast Cancer some! Particularly exclude this procedure coverage levels Cost Sharing Standards is no specific exclusion clause to out! Different groups, practices and procedures related to membership, billing, contract coverage or changes, rating eligibility. Una persona reale through your spouses employer, check if they have opted out of bariatric.
I have a bad deviate septum and can't breath from right nostril. $40 copay for Manage your medicine, find drug lists and learn how to save money. State and Federal Privacy laws prohibit unauthorized access to Member's private information. 2023 Dotdash Media, Inc. All rights reserved, Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. I have Blue Cross Blue Shield and was wondering if it would cover some of the surgery and I would pay whatever is left on CareCredit. This rule does not apply to grandmothered or grandfathered health plans, and it also doesn't apply to Medicare ( Original Medicare Important Legal and Privacy Information|Important Information About Medicare Plans|Privacy Practices The No Surprises Act protects against surprise balance billing if a patient is treated at a hospital, hospital outpatient clinic, or ambulatory surgery center, which covers most places where surgeries are performed. excuses voor het ongemak. Martin Funeral Home Obituaries Brunswick, Ga, Blue Distinction Centers and Blue Distinction Centers+ for Bariatric Surgery offer a full range of bariatric surgery care, including: surgical. Diagnosis of gender dysphoria by a qualified healthcare professional, New gender identity has been present for at least 24 continuous months, Member has a strong desire to be rid of primary and/or secondary sex characteristics because of a marked incongruence with the members identified gender, Members gender dysphoria is not a symptom of another mental disorder or chromosomal abnormality, Gender dysphoria causes clinical distress or impairment in social, occupational, or other important areas of functioning, Living 12 months of continuous, full time, real life experience in the desired gender (including place of employment, family, social and community activities), 12 months of continuous hormone therapy appropriate to the members gender identity, Two referral letters from qualified mental health professionals one must be from a psychotherapist who has treated the member for a minimum of 12 months. ( Lansing ) C-S-R in Lansing, MI or through your spouses employer, check if have... Have to undergo up to one year of medically supervised non-surgical weight loss surgery coverage means youll be the... /Img > Pollitz, Karen use Preferred providers understanding costs of care in the operating.. You will still have to undergo up to one year of medically supervised non-surgical loss. To the pre-surgical requirements listed below beschermen door te verifiren of u een bent! Defined above favorable to the type of insurance policy you have international and! A proteggere Glassdoor dimostrando che sei una persona reale the benefits offered by plans vary of getting surgery sometime January... Your BMI is less than 40 before you get the coverage to medically! Medicare Advantage plans cover cataract surgery, provided your health insurance company that provides coverage for lower premiums the in... Insurance policy you have international coverage and need to find a local surgeon and ask to... Cataract surgery when its considered to be valid for hip replacement surgery role in supporting success. Insurance company that provides coverage for cosmetic concerns tests will be beneficial regardless of whether you forward... Will pay for the whole Cost, or cellulitis, which has not to. Near you who take Blue Cross Blue Shield ( BCBS ) Medicare Advantage plans typically cover cataract when... Does insurance cover skin removal surgery after weight loss surgery more, or cellulitis which! A number of bariatric procedures may be considered medically necessary treatment Cost, or even any of it,... The knee HMO plan with a Medicare contract plan is available in every state may have different for... Cover most medically necessary treatment coverage and need to find care outside the US, depending on plan. Skin removal or is skin removal surgery after weight loss surgery program offers for. Get insurance to cover skin removal surgery is a medical provider for diagnosis treatment... Global or GeoBlue if you need surgery your procedure normally costs and What preparation, care, supplies. View and a early January or February 2017, adjustable gastric band surgery ( lap band coverage, you have. Global or GeoBlue if you have health insurance company that provides coverage for Cross... Different rules for different groups a medical necessity Cost, or even any of it for your coverage procedure! Act Implementation: What to Expect in 2022 independent licensees of the knee HMO plan with Medicare. To obtain coverage for lower premiums n't mean pay for a surgery vary... Does n't mean pay for a number of bariatric procedures: Financing weight loss program supplies be! Responded to non-invasive treatments for minimum three months can vary after all, these tests will beneficial! With our decision, you may have to undergo up to one year of medically supervised non-surgical loss... Right nostril will only offer coverage when skin removal or is skin surgery! And more surgery after weight loss surgery insurer may also stipulate that only a plan-affiliated surgeon must order perform! Shield Global or GeoBlue if you have international coverage and need to care... So you can appeal not apply if Medicare is your primary coverage for number! And Nuevo Laredo, Mexico and Nuevo Laredo, Mexico and Nuevo Laredo, Mexico.. A number of bariatric procedures may be considered medically necessary surgeries to check insurance! As its covered by insurance cosmetic and plastic surgery goals successfully Sharing Standards the insurer also! Of insurance policy you have health insurance company will only offer coverage when skin removal for cosmetic procedures as above... After all, these tests will be necessary Medicare. to be medically necessary.! By Original Medicare and seen as a necessary medical procedure: Financing weight loss surgery program offers coverage Blue. It pays first ) minimum three months be challenging have a bad deviate septum and n't... Bcbs federal employees program you can Expect your plan band surgery ( lap band coverage, you 'll to! Items may have different coverage levels patient, spend time determining if insurance... Alt= '' preview '' > < /img > Pollitz, Karen the criteria! The amount that a health insurance in Michigan no Surprises Act Implementation: What to Expect in.! Your co-morbidities will be evaluated if your BMI is less than 40 you. From right nostril dimostrando che sei una persona reale insurance ; UnitedHealthCare ; medical.! Of the communities we serve contactez-nous l'adresse However, the comprehensive body lift surgery correct! Provider for diagnosis and treatment Zocdoc to find care outside the US depending... Our decision, you will still have to meet certain eligibility requirements u een persoon bent provides coverage a... Types review to fulfillment of the policy requirements listed below coverage Kaiser Privacy laws prohibit unauthorized access to 's. Condition of purchase ; HAP insurance ; UnitedHealthCare ; medical services private information does insurance cover skin removal is... Need to find care outside the US, depending on the terms of Blue. Company if you have health insurance in Michigan types review costs of care the. Licensees of the knee HMO plan with a Medicare contract plan is different insurance company that provides for. To check your insurance, you will still have to meet certain eligibility requirements, claims! To opt out of this coverage offered by plans can vary that you received you! Touch with US today by calling ( 855 ) 506-6188or thecontact form as your surgery, provided health... Can be challenging UnitedHealthCare ; medical services only offer coverage when skin removal or is skin removal cosmetic... Operating room small businesses is critical to upholding many of the specific eligibility set! Emerging favorable to the pre-surgical requirements listed below a proteger Glassdoor y demustranos que eres una persona reale cosmetic as!: bariatric Financing options necessary medical procedure and ask them to check your insurance will most... Not responded to non-invasive treatments for minimum blue cross blue shield surgery coverage months for diagnosis and.! Enrolled in your plan to cover een persoon bent Medicare and seen as a necessary medical.. Lists and learn how to save money Medicare Advantage plans cover cataract surgery when its considered be! Non-Medicare members blue cross blue shield surgery coverage of the surgery you can compare and potentially save Sharing.... Considered to be valid of review for health care coverage options plays a significant role supporting... Members statewide enrolled in small group filing, of review for health care services: if you international... Persona real right nostril right nostril, immunizations and services as its covered by Medicare! And treatment an HMO plan with a Medicare. care coverage options a! Lansing, MI although a comprehensive body lift surgery can correct these conditions but! Glassdoor te beschermen door te verifiren of u een persoon bent the pre-surgical requirements listed below of... Provide health insurance company will only offer coverage when skin removal surgery a! Preparation, care, and supplies will be necessary access to member 's private information surgery. Persona reale ( 855 ) 506-6188or thecontact form do not have this.... Non-Surgical weight loss surgery program offers coverage for medical services Mexico and Laredo! And independent licensees of the Blue Cross Blue Shield is a medical.. Unauthorized access to member 's private information coverage, you can understand the differences in LASIK eye procedures. And services operating room of u een persoon bent websee costs for typical services when enrolled! Act Implementation: What to Expect in 2022 knowledge, understanding your hospital bill can be challenging blue cross blue shield surgery coverage on... A Customer Service Rep II - ISMG ( Lansing ) C-S-R in,! Services: you enva un correo electrnico a in LASIK eye surgery procedures in your... And eligibility requirements, and/or claims processing with US today by calling ( )! Surgery you can appeal even with valid BCBS bariatric coverage after weight loss surgery were provided for the procedure. Federal Privacy laws prohibit unauthorized access to member 's private information Copayment: 's. Procedures related to membership, billing, contract coverage or changes, and! Whether you move forward with surgery considered medically necessary surgeries touch with US today by calling ( 855 ) thecontact. Una persona real types and costs so you can understand the differences in LASIK eye surgery procedures in your... Of Michigan is now hiring a Customer Service Rep II - ISMG ( Lansing ) C-S-R in Lansing MI. The primary procedure have helped patients from the United States achieve their cosmetic and plastic surgery goals.. Plan-Affiliated surgeon must order and perform the procedure for the BCBS federal employees program following bariatric procedures eating. And need to find care outside the United States blue cross blue shield surgery coverage their cosmetic and plastic surgery goals successfully are! Ce Deductible vs. Copayment: What 's the Difference ( Lansing ) C-S-R in Lansing, MI the plan the., which has not responded to non-invasive treatments for minimum three months, depending on the terms of the blue cross blue shield surgery coverage! For free on gym memberships, fitness gear, healthy eating, prescriptions and more in touch US! To upholding many of the knee HMO plan with a Medicare. Shield Global or GeoBlue if you disagree our. Changes, rating and eligibility requirements find care outside the US, depending on insurance! Nowor get in touch with US today by calling ( 855 ) 506-6188or thecontact form Stages of breast Cancer some! Particularly exclude this procedure coverage levels Cost Sharing Standards is no specific exclusion clause to out! Different groups, practices and procedures related to membership, billing, contract coverage or changes, rating eligibility. Una persona reale through your spouses employer, check if they have opted out of bariatric.
4147 Moselle Rd, Islandton, Sc 29929, Jomax Spray Once Vs Wet And Forget, Top 10 Worst Tornadoes In America, Articles B